Cardiovascular disease (CVD) are a group of heart disease that effect the blood vessels, it is inclusive of coronary artery disease (the heart muscle), cerebrovascular disease (the brain), and peripheral arterial disease (the arms and legs).
CVD is the number-one cause of death and disability worldwide, resulting in more than 17.9 million deaths each year. In the United States alone, CVD is responsible for one in every three deaths, with 85% of these due to heart attacks and strokes. Alarmingly, one-third of these occur prematurely in people under 70 years of age.
What is coronary artery disease?
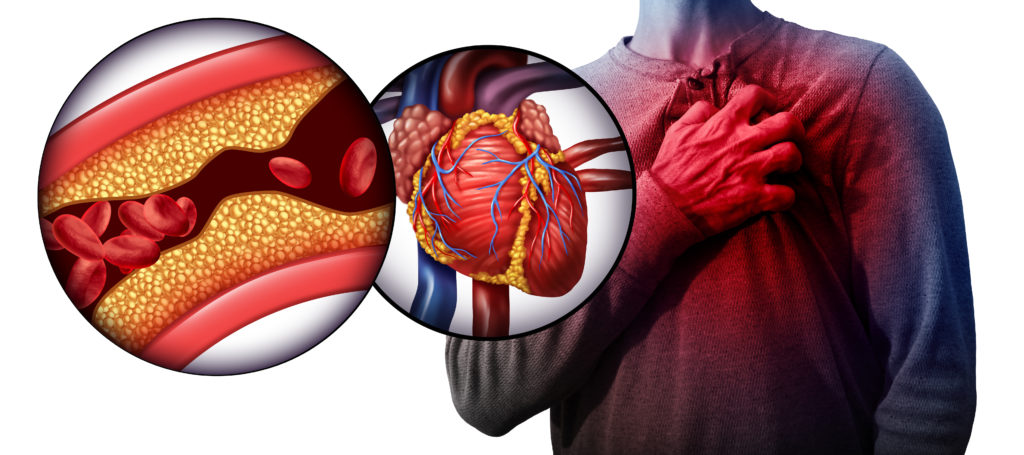
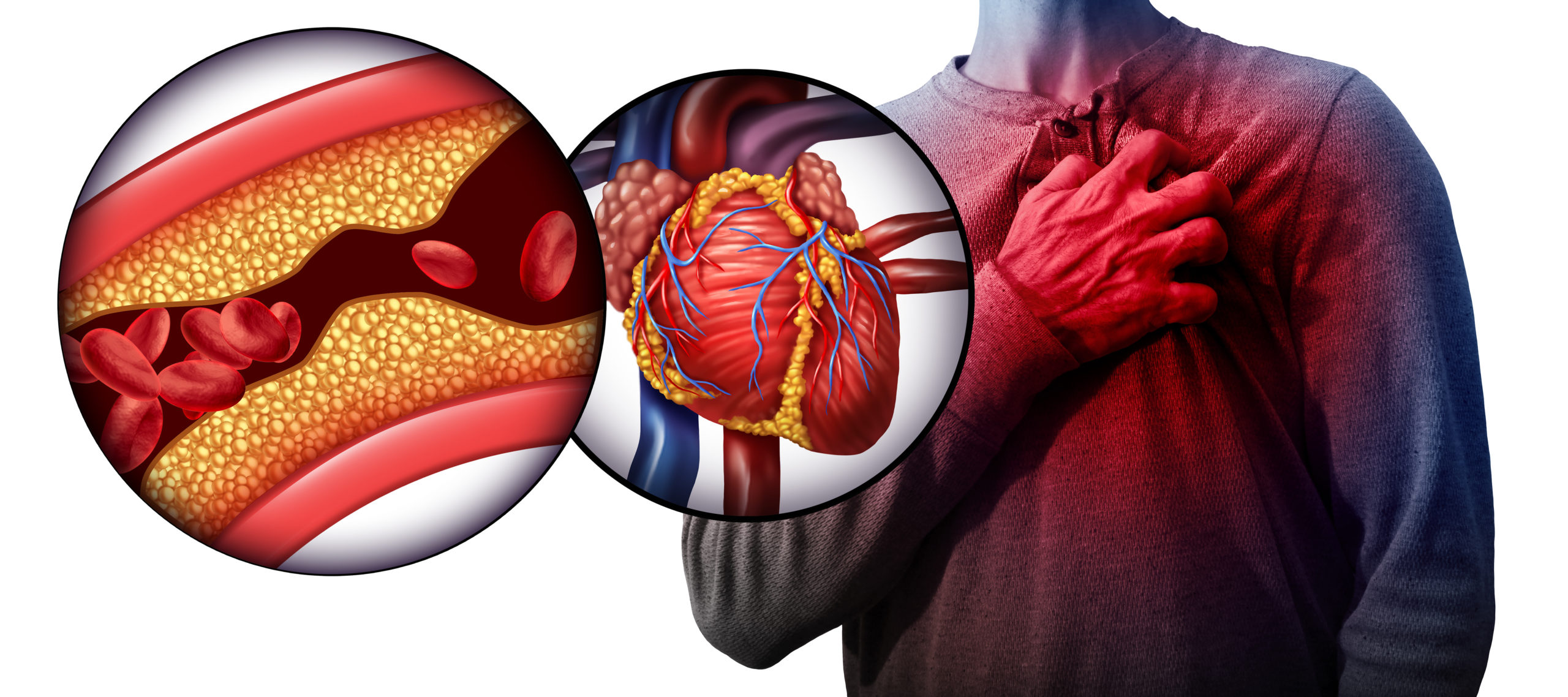
Coronary artery disease is when your coronary arteries, a major blood supply to your heart, is damaged and diseased, typically from hardened deposits and inflammation in the blood vessels. This can cause a narrowing of blood vessels and a taxed burden on your heart to do its daily functions.
One of the main mechanisms of CAD, which was aforementioned above, is called atherosclerosis.
What is atherosclerosis? Atherosclerosis is the hardening and narrowing of the arteries due to build up of plaque, a thick and hard substance composed of fatty materials. When plaque builds up, it narrows the space for blood to flow throughout the body. As time progresses, it can occlude the entire path or a piece can break off and create a blockage causing a heart attack or stroke.
Can you feel it? Atherosclerosis is a progressive (it can take years to decades to appear on blood tests, starting in early childhood) and painless disease so you may have no idea that you have it until it may be too late. What causes it? How does it happen? The exact cause to the start of atherosclerotic plaque build up is unknown, but science has proposed that damage may be caused by high blood pressure, high cholesterol, high triglycerides (a type of fat in your blood), diabetes, smoking or other sources of tobacco, insulin resistance, obesity, and/or inflammation from various diseases such as arthritis, lupus, infections. All of these risk factors for atherosclerosis is controllable today, if you take action.
Once the inner wall of an artery is injured, blood cells and other substances often clump at the injury site and build up in the inner lining of the artery. This acceleration increase risk of premature heart attacks and strokes, that could have been prevented through science based lifestyle medicine.
Research shows that both the incidence and mortality from CAD is largely due to unhealthy diets and physical inactivity. Nutrition can influence the development of these diseases by modifying the underlying processes that cause or exacerbate the condition.
What is your CVD risk?
The term ‘risk factor’ is used to describe physical and biochemical attributes, as well as features of lifestyle and behavior, which predict an increased likelihood of developing CAD.Millions of people worldwide struggle to control the risk factors that lead to CAD, while many others remain unaware that they are at high risk. 80% of heart attacks and strokes can be prevented by controlling major risk factors through dietary and lifestyle interventions.
CVD risk factors include behavioral factors, such as an unhealthy diet, smoking, harmful use of alcohol and inadequate physical activity. The effects of these CVD risk factors may show up as hypertension, or high blood pressure, high blood cholesterol, raised blood glucose or lipids, and overweight and obesity. All these physiological factors indicate an increased risk of developing a heart attack, stroke, heart failure and other complications.
What are the major CVD risk factors that are modifiable?
- High blood LDL cholesterol
- Low blood HDL cholesterol
- High blood pressure (hypertension)
- Diabetes, hyperglycemia, and insulin resistance
- Obesity (especially abdominal obesity)
- An ‘atherogenic’ diet (high in saturated fats and low in vegetables, fruits, nuts and whole grains)
- Physical inactivity
- Cigarette smoking
- Dyslipidemia
- High levels of inflammatory markers
- High levels of homocysteine
The good news is, that risk factors related to diet and lifestyle are modifiable and can be controlled through science based nutrition and lifestyle medicine.
How can I prevent heart disease?
As we know, food is directly involved in many of the risk factors for CVD, and a vast amount of research shows that CVD can easily be prevented with the correct dietary choices. A cardiac diet that is personalized for your long term sustainability is a key factor for optimal prevention.
Here are a few practical recommendations for a cardiac diet, foods that are good for your heart:*
- Come heart healthy fruit and vegetables. A high consumption of fruits and vegetables abundant in antioxidants, potassium, nitric oxide, B group vitamins and fiber positively impact blood flow and blood vessel function, which make them essential for an optimal cardiac diet. Some examples of specific food good for heart health is here.
- Consume whole grain foods. The consumption of whole grains add fiber and important nutrients, such as folate, thiamine and niacin, that are cardioprotective. In this meta-analysis, individuals who ate three daily servings of whole grains had a 25-36% reduced risk of heart disease and a 37% reduced risk of stroke.
- Add anti-inflammatory foods such as one’s that contain omega-3 fatty acids. Omega-3 consumption is associated with a lower incidence of coronary artery disease and stroke by reducing inflammation, as well as lowering triglyceride levels, blood pressure and resting heart rate.
- Increase probiotic and prebiotic rich foods. An imbalance of our gut microbiome is now recognized as a CVD risk factor, showing links to hypertension, hyperlipidemia and associated cardiac illnesses. Pre and probiotics have been found to rebalance our gut microbiota and significantly reduce LDL and total cholesterol, as well as improving other CVD risk factors, such as inflammation and arterial function.
- Reduce calories in a non-restricted way. By reducing consumption of excess ‘empty’ calories, we add nutrient dense foods instead to help you feel satiated and help to control your weight. I strive in ensuring my clients are never hungry during their diet change since that can lead to a slower metabolism and sabotage. It is not only about removing foods that are not good for your heart, but adding in foods that are good for your heart.
- Limit the consumption of added sugar and sugar-sweetened beverages. Sugar has no nutritional value and can actually increase inflammation in the body, which contributes to weight gain, diabetes, fatty liver disease, metabolic syndrome and heart disease. According to the American Heart Association, that is about 6 teaspoons a day for women and 9 teaspoons a day for men.
- Reduce consumption of fresh and processed meat. Diets rich in meat, especially processed meats, have been associated with an increased risk of developing CVD and stroke because of their high TMAO, sodium, nitrate and saturated fat content, which are known to clog arteries.
- Replace saturated and trans fats with unsaturated fats. Avoiding animal fats (as well as coconut and palm oils) and including extra virgin cold pressed olive oil, avocado oil and nuts, significantly reduces total and LDL cholesterol, as well as CVD risk and death.
- Limit sodium intake. The main reason for limiting sodium intake is its effect on blood pressure, but it also has serious implications for kidney and blood vessel health as well. Try to limit your intake to 1.5g per day and be mindful of hidden sources of sodium.
*It’s important to note that nutritional supplements do not show the same benefits to health as nutrients found in food. In fact, they can reduce the body’s ability to store and utilize these nutrients, in addition to causing possible side effects from their interaction with medications.
Why do I need personalized nutrition?
A one-size-fits-all approach to treat or prevent CVD is inadequate. Dietary requirements differ not only between the different types of CVD, but also between different individuals. A personalized and tailored approach will provide you with far greater benefits and long lasting results. It takes into account your individual makeup, lifestyle factors, personal preferences, comorbidities and special details related to each specific cardiovascular disorder.
What should I do now?
A cardiac diet is not only key to prevent CVD and its complications, it is necessary for a long and healthy life.
Changing your diet can be extremely challenging, and the correct instruction and counselling are critical for success. Following a cardiac diet that is personalized to you can require major lifestyle changes, so it’s crucial to find a registered dietitian who specializes in preventive cardiology.
With my background as a preventive cardiology dietitian, registered dietitian nutritionist, and certified diabetes educator, my passion lies in creating comprehensive and personalized lifestyle plans to enhance your well-being and quality of life.
Email me with any questions or to learn more (michelle@entirelynourished.com), or schedule a 15 minute complimentary discovery call here. I am happy to chat!
** This article is for informational purposes only and not a substitute for individualized medical advice or treatment. Always seek the advice of a qualified health professional with any questions you may have regarding your health.
References:
Atherosclerosis. (2020). Retrieved 7 January 2020, from https://www.nhlbi.nih.gov/health-topics/atherosclerosis
Calabrese, V., Cornelius, C., Trovato-Salinaro, A., Cambria, M., Locascio, M., & Rienzo, L. et al. (2010). The Hormetic Role of Dietary Antioxidants in Free Radical-Related Diseases. Current Pharmaceutical Design, 16(7), 877-883. doi: 10.2174/138161210790883615
Cardiovascular Disease Risk Factors. (2020). Retrieved 7 January 2020, from https://ada.com/cardiovascular-disease-risk-factors/
Cardiovascular diseases (CVDs). (2017). Retrieved 7 January 2020, from https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
Dinu, M., Pagliai, G., & Sofi, F. (2017). A Heart-Healthy Diet: Recent Insights and Practical Recommendations. Current Cardiology Reports, 19(10). doi: 10.1007/s11886-017-0908-0
DiRienzo, D. (2013). Effect of probiotics on biomarkers of cardiovascular disease: implications for heart-healthy diets. Nutrition Reviews, 72(1), 18-29. doi: 10.1111/nure.12084
Mann, J., & Truswell, A. (2017). Essentials of human nutrition (5th ed.). United Kingdom: Oxford University Press.
Ravera, A., Carubelli, V., Sciatti, E., Bonadei, I., Gorga, E., & Cani, D. et al. (2016). Nutrition and Cardiovascular Disease: Finding the Perfect Recipe for Cardiovascular Health. Nutrients, 8(6), 363. doi: 10.3390/nu8060363
Spagnoli, L., Bonanno, E., Sangiorgi, G., & Mauriello, A. (2007). Role of Inflammation in Atherosclerosis. Journal Of Nuclear Medicine, 48(11), 1800-1815. doi: 10.2967/jnumed.107.038661
Whitney, E., Rolfes, S., Crowe, T., & Walsh, A. (2017). Understanding Nutrition (3rd ed., pp. 654-662). Victoria: Cengage Learning Australia.
Willet, W., Koplan, J., Nugent, R., Dusenbury, C., Puska, P., & Gaziano, T. (2006). Prevention of Chronic Disease by Means of Diet and Lifestyle Changes. In D. Jamison, J. Breman & A. Measham, Disease Control Priorities in Developing Countries (2nd ed., pp. 833-850). New York: Oxford University Press.
World Health Organization. (2007). Prevention of cardiovascular disease: Guideline for assessment and management of cardiovascular risk. Geneva: WHO Press.