What causes plaque in arteries? It’s a question more people should be asking, especially since it’s the underlying cause of about 50% of deaths in Westernized society.
Plaque often develops silently for years, which is why understanding how and why it forms is one of the most important steps you can take to protect your heart.
And guess what… You can actually shrink one of the types of plaque we’ll be talking about today. So if you have some plaque buildup already, you’re absolutely in the right place.
In this blog, we’ll break down what plaque buildup is, why it matters, and the major factors that drive it.
Interested in 1:1 personalized nutrition counseling? Book a free discovery call today to learn more about how we can work together to reduce plaque buildup through targeted science backed nutrition and lifestyle changes.
What is Plaque Buildup in Arteries?
Before diving into what plaque buildup is and what causes plaque in arteries, there are a couple of key terms to understand.
- Plaque: A substance made up of a mix of fat, calcium, cholesterol, and other substances in your bloodstream.
- Atherosclerosis: The name of the disease that occurs when plaque builds up in your arteries.
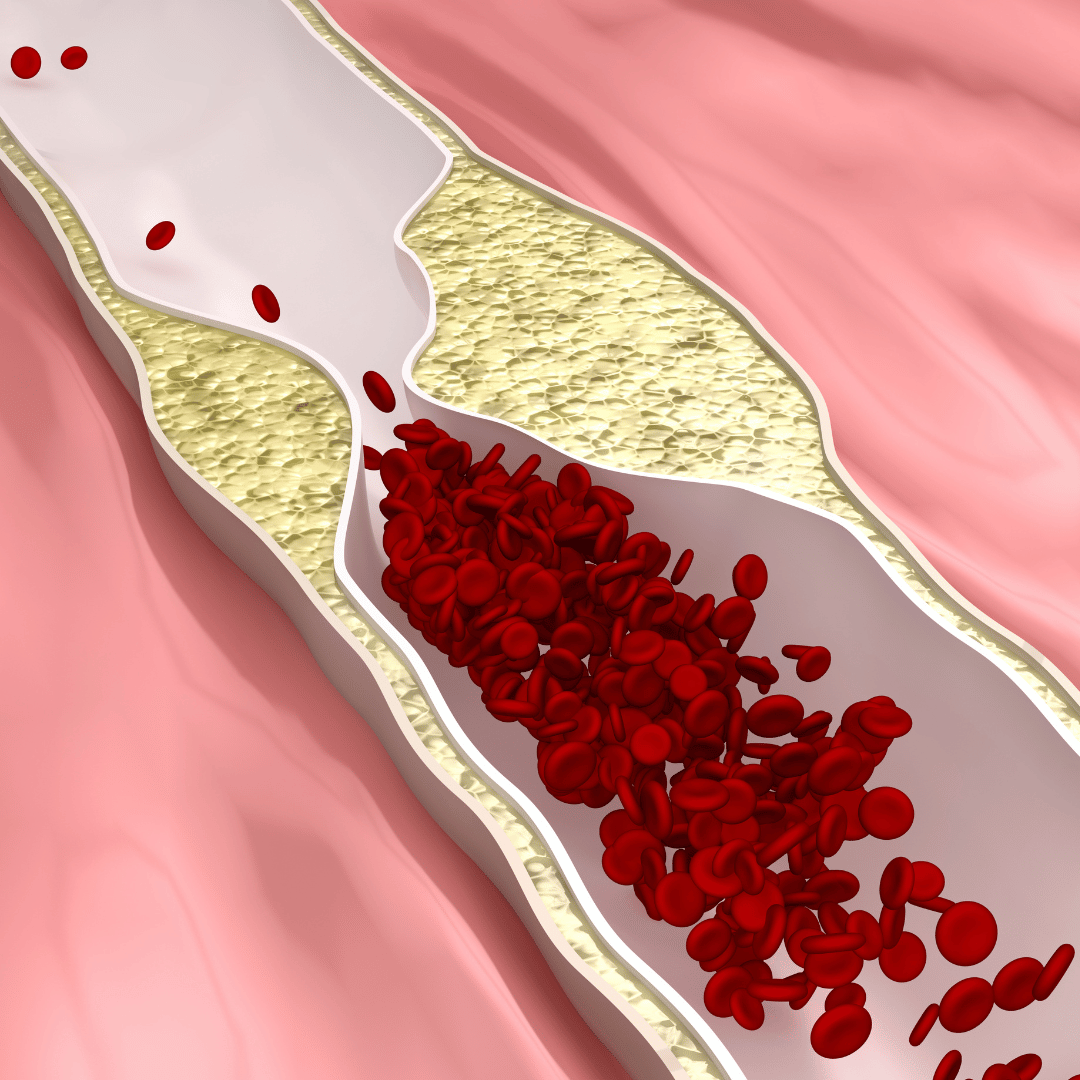
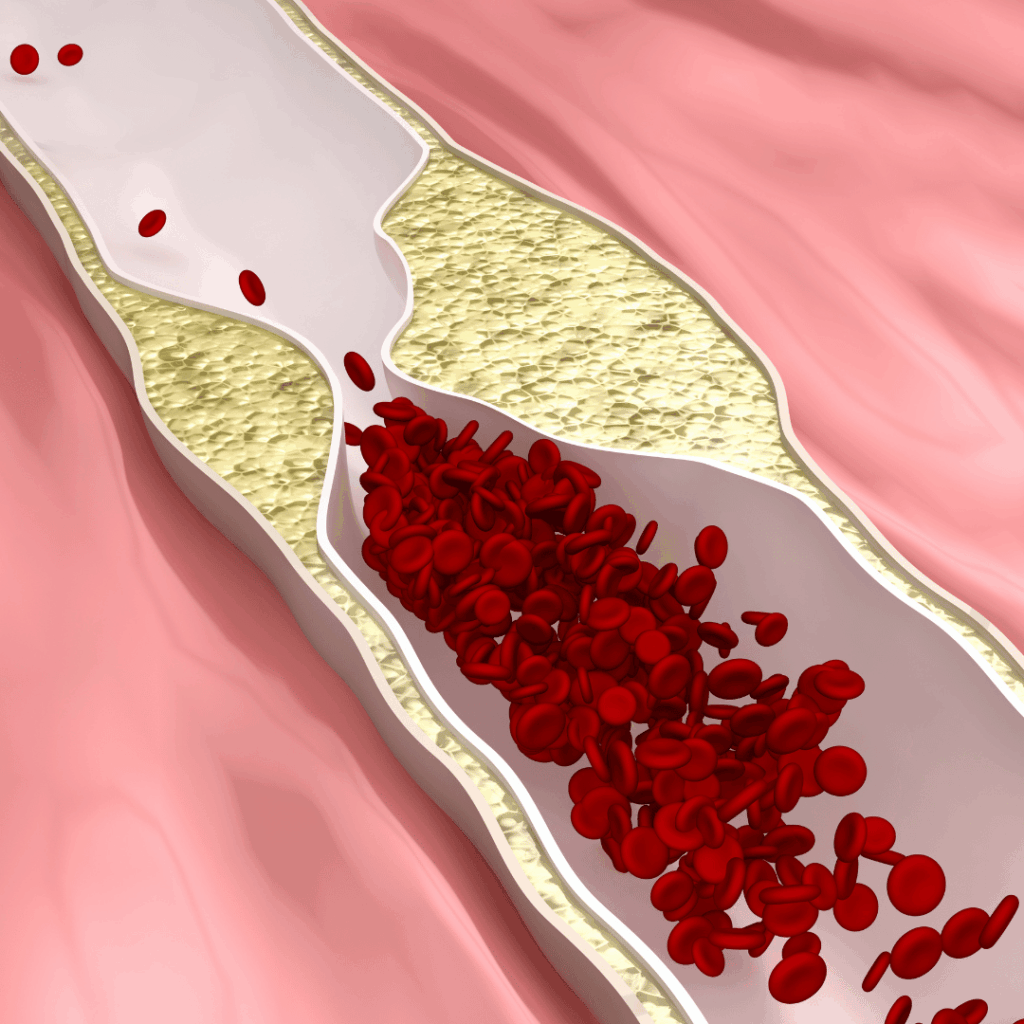
Over time, the buildup of plaque thickens and narrows the arteries, which slows blood flow to organs like your heart, brain, and kidneys. Because of this, your heart has to work harder, which puts you at an increased risk for complications such as a heart attack, stroke, heart failure, kidney disease, and dementia.
There are two types of plaque buildup:
- Soft plaque: This type of plaque is a fatty, cholesterol-rich buildup that’s unstable and more likely to rupture, which can cause clots, heart attack, or stroke. With this type of plaque, we can actually regress and shrink it through targeted science-backed nutrition and lifestyle changes.
- Hard plaque: This type of plaque is older and has hardened with calcium. This makes it more stable, but it does narrow and stiffen the arteries.
There are many arteries in the body in which plaque can build up. It’s a whole body process, that’s not just directly tied to your heart.
- Coronary arteries: This is the most common location for plaque buildup. Buildup here can lead to chest pain, a heart attack, or heart failure. The function of the coronary arteries is to provide blood to the heart.
How to Detect Hardened Plaque
To detect the buildup of hardened plaque in your coronary arteries, you can use a calcium score heart scan. It’s a heart screening test used to detect calcium deposits in your coronary arteries and help you understand if you’re at an increased risk of having a heart attack.
- Carotid arteries: These arteries carry blood to your brain. Plaque buildup in this location can limit blood flow or cause a clot, which can lead to further complications such as a stroke or memory issues.
- Renal arteries. The function of these arteries is to bring blood to your kidneys, which is essential for filtering waste, balancing fluids, and controlling blood pressure. When plaque builds up here, it can increase blood pressure and contribute to chronic kidney disease.
- Femoral arteries: These arteries run down your legs, bringing oxygen to your skin and muscles. Buildup here is known as peripheral artery disease (PAD), which causes cramps and leg pain.
Plaque buildup is a full-body condition that affects how efficiently your organs receive the oxygen and nutrients they need to function optimally. Understanding what plaque buildup is is the first step to protecting your heart health and reducing your risk of long-term complications.
How Does Plaque Form in the Arteries?
Here’s how the plaque formation process works:
- The artery lining gets irritated: Constant stress can damage the inner lining of your arteries, making it easier for cholesterol to stick where it shouldn’t.
- More inflammation and unhealthy cholesterol buildup: Stress increases inflammation and can raise harmful cholesterol levels. This makes it easier for cholesterol to collect inside the artery wall.
- Cholesterol gets trapped and forms “foam cells”: Immune cells try to clean up the cholesterol but end up filling with it. These foam cells are the start of plaque.
- Plaque grows and may block the artery: Over time, the plaque gets bigger and harder, narrowing the artery. If a plaque breaks open, it can cause a heart attack or stroke.
Why Plaque Buildup Matters for Your Health
Plaque buildup in your arteries can lead to complications. These are the most common health problems that atherosclerosis can cause:
- Heart attacks: When plaque blocks blood flow to your heart, it can lead to a heart attack.
- Heart failure: Over time, limited blood flow due to plaque buildup can cause the heart to no longer pump blood well, leading to heart failure.
- Stroke: Plaque in the arteries that deliver blood to the brain can lead to the formation of a clot, which can cause a stroke or a transient ischemic attack (a “mini-stroke”). Additionally, plaque can break off and travel to the brain, leading to the sudden blockage of blood flow.
- Dementia: Plaque buildup in the arteries that supply your brain can limit blood flow and damage brain tissue over time, raising the risk of vascular dementia, a type of dementia caused by problems with the brain’s blood vessels.
- Kidney failure: When plaque blocks the arteries that carry blood to the kidneys, the kidneys can’t filter waste effectively, which can lead to chronic kidney disease.
- Peripheral artery disease: A decrease in blood flow in your leg arteries can cause leg pain, slow-healing wounds, and infections.
Early detection of plaque buildup is key because identifying plaque buildup before it causes blockages gives you the best chance to prevent these complications.
What Causes Plaque in Arteries? 10 Main Causes
Now that you understand what plaque buildup is and why it matters for your health, it’s important to understand what causes plaque in arteries.
1. Age and Sex
Age: As you get older, your arteries naturally become stiffer and more likely to collect calcium. This makes it easier for plaque to form and harder for your blood vessels to function normally.
Sex: Men usually develop plaque earlier in life, while women tend to see their risk rise after menopause because estrogen levels drop. This hormonal shift is complex and affects cholesterol, inflammation, and vascular function in many ways.
It is important to note that hormone replacement therapy is individualized and currently used only for symptom relief, not for preventing or treating cardiovascular disease. Because of these changes, nutrition and lifestyle strategies often need to be more targeted and personalized during the menopause transition and beyond.
2. Genetics and Family History
Certain inherited traits can affect the way your body processes fats and cholesterol. Conditions like familial hypercholesterolemia, elevated Lp(a), or carrying an APOE4 variant can raise LDL levels or make the arteries more sensitive to inflammation, which increases the chance of plaque buildup.
But genetics only create a predisposition; they don’t predetermine your future. Many people with a strong family history never develop heart disease when other risk factors are well managed.
If heart disease runs in your family, it can be helpful to ask your clinician about screening tests like Lp(a) and apoB, which give a clearer picture of inherited lipid-related risk and can guide more personalized prevention strategies. Plaque development can occur at lower thresholds, so being proactive is a great way to make sure your heart is staying healthy.
3. High Blood Pressure
When looking at what causes plaque in arteries, another factor that contributes is high blood pressure (hypertension).
Here’s how it works:
- High blood pressure puts constant force on the artery walls, creating tiny microtears in the lining.
- These microtears make it easier for LDL and apoB-containing particles to slip inside, where they become oxidized and trigger inflammation.
- This starts the multistep plaque formation process.
- Ongoing high pressure continues to stress the artery, allowing plaque to grow faster and making it more likely to rupture.
4. LDL Cholesterol and ApoB
Cholesterol travels through your blood through tiny particles called lipoproteins. Some lipoproteins protect your arteries, and some can cause plaque buildup.
Here’s a breakdown:
LDL (“bad” cholesterol): Its function is to carry cholesterol from your liver to other tissues and cells in the body. Too many LDL particles can lead to them slipping into your artery wall. Once inside, they can become oxidized and trigger inflammation, leading to the formation of plaque.
HDL (“good” cholesterol): Its job is to help clear extra cholesterol from your arteries and bring it back to the liver to be removed. Our goal is to support healthy HDL function, not just raise the number on your lab report.
apoB: The apoB marker gives you a true count of all the cholesterol-carrying particles that can cause plaque (LDL, VLDL, and IDL) because each one carries exactly one apoB molecule. That’s why apoB is often a more accurate way to measure the number of atherogenic (plaque-forming) particles in your blood, even when your LDL cholesterol level looks normal.
Even if your LDL numbers are in the normal range, a high apoB can mean you still have too many plaque-causing particles circulating, which indicates a higher risk for plaque buildup.
5. Smoking and Toxin Exposure
Smoking and toxin exposure are two additional factors of what causes plaque in arteries.
Smoking: Smoking contributes to the formation of plaque by damaging the lining of your arteries, which makes it easier for cholesterol-carrying particles to get into the artery wall. Additionally, it increases inflammation and oxidative stress in the blood, accelerating the growth of plaque.
Toxin Exposure: Many environmental toxins and pollutants can speed up plaque formation by damaging blood vessels and worsening traditional risk factors. One example is PFAS, also known as “forever chemicals,” which increase oxidative stress and inflammation, leading to injured arterial linings, increased blood pressure and cholesterol, and the buildup of plaque.
6. Poor Diet
A poor-quality diet can speed up atherosclerosis by tipping the balance toward high LDL and causing more inflammation.
- Diets high in saturated or processed foods raise LDL and apoB, which makes plaque formation more likely.
- Low-antioxidant diets increase oxidized LDL, a key driver of artery damage.
- Not getting enough anti-inflammatory nutrients (like omega-3s and polyphenols) worsens inflammation and endothelial injury (damaged blood vessel lining).
7. Lack of Physical Activity
Not getting enough physical activity is strongly linked to a higher risk of atherosclerosis. There are several ways inactivity can contribute to plaque buildup:
- Worsens major risk factors like higher blood pressure, elevated blood sugar, and weight gain.
- Lowers overall fitness, which is linked to significantly higher rates of heart disease.
- Heightens inflammation and oxidative stress, which allows more damage to your artery linings.
- Less movement weakens endothelial function.
- Long periods of muscle inactivity reduce circulation, slow metabolism, and increase cardiovascular risk.
8. Chronic Stress
Chronic stress is another contributor to what causes plaque in the arteries.
Stress affects more than your mood. It often leads to poorer sleep, less movement, and more convenience-based food choices, which can raise risk factors like high blood pressure, inflammation, and elevated LDL.
Stress hormones also increase insulin levels and make blood sugar harder to control. Over time, this combination of higher insulin, more inflammation, and less supportive lifestyle habits creates an environment where plaque can form more easily.
9. Inflammation
Inflammation acts like a constant alarm signal in your body. Your artery walls keep calling in immune cells, which stick to the irritated lining, move inside, and turn into foam cells that form early fatty streaks, the first step in plaque development.
Over time, these immune cells release more inflammatory chemicals, pulling in even more immune cells and helping build the thick, fibrous plaque that gradually narrows the artery.
Chronic inflammatory conditions that are not well controlled, like psoriasis, eczema, rheumatoid arthritis, diverticulitis, and other autoimmune or inflammatory diseases, can keep inflammation elevated long-term, which raises the risk of heart disease and accelerates plaque formation.
10. Diabetes or Insulin Resistance
Diabetes and insulin resistance make the arteries more vulnerable to plaque by disrupting the way the body handles both glucose and lipids, making it a key contributor in what causes plaque in arteries.
When blood sugar is consistently high, it leads to the formation of advanced glycation end products (AGEs) that irritate the artery lining, making it easier for LDL particles to get trapped and keep inflammation high.
At the same time, insulin resistance promotes a more atherogenic lipid pattern, including small dense LDL that’s more easily taken up by foam cells.
These changes happen together, and they affect nearly every step of plaque formation. People with diabetes are at risk of developing atherosclerosis earlier.
How to Reverse Plaque in Arteries
Now that you understand what causes plaque in arteries, I have some good news for you.
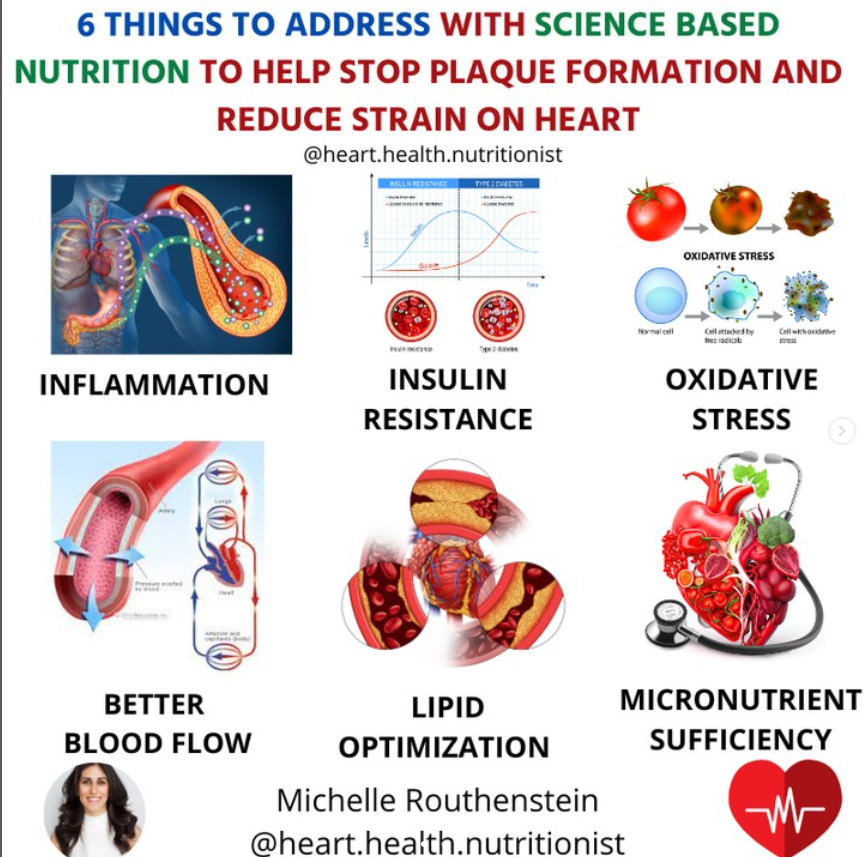
The encouraging news is that soft plaque can regress with the right lifestyle habits. While fully calcified plaque typically stays in place, it can still become unstable in certain situations. When you know you have plaque in your arteries, the goal is to stabilize hard plaque along the outer edges of the artery wall and shrink soft plaque away from the lumen (the middle area where blood flows) through targeted, nutrient-adequate nutrition. These changes help lower inflammation, improve lipids, support the arterial lining, and reduce overall cardiovascular risk.
Core strategies that help reduce and stabilize plaque include:
- Eating a fiber- and antioxidant-rich diet to lower inflammation and support healthy cholesterol levels.
- Balancing omega-3 and omega-6 fats through more fish, nuts, seeds, and fewer highly processed oils.
- Keeping apoB in a healthy range <90mg/dL for no risk, <70mg/dL for moderate <60mg/dL for high
- Managing blood pressure, stress, and blood sugar, since all three directly affect artery health.
- Quitting smoking and limiting alcohol, which reduces oxidative stress and vascular injury.
- Exercising regularly and prioritizing restorative sleep, both of which protect the endothelium and help your body repair.
Tracking Progress
To track progress in your coronary arteries specifically, you can use a coronary calcium score, which looks only at calcified (hard) plaque in the coronary arteries. It does not measure soft plaque. If you need a test that evaluates both soft and hard plaque, a coronary CT angiography (CCTA) provides a more complete picture of plaque type and location.
Some people need medication to reach safe lipid levels. These tools work alongside nutrition and lifestyle, not instead of them. Lifestyle habits are the foundation for long-term heart health.
Through personalized nutrition, I have helped hundreds of clients stabilize hard plaque and shrink soft plaque on CCTA in my private practice as a cardiovascular dietitian. If you’re looking for support, I’d be happy to help you, too. You can learn more about working together here!
FAQs: What Causes Plaque in Arteries?
What foods cause plaque buildup in arteries?
These foods can increase inflammation, raise LDL and apoB levels, and contribute to insulin resistance, all of which make it easier for plaque to form in the arteries.
- Trans fats (fried fast food, packaged pastries).
- Processed meats like bacon, sausage, hot dogs.
- Sugary foods and refined carbs (soda, candy, white bread).
- Deep-fried foods that produce oxidized fats.
- Ultra-processed snacks (chips, packaged sweets, fast food).
What causes calcium buildup in arteries?
Calcium buildup happens when existing plaque has been in the artery wall for a long time, and the body tries to stabilize it by hardening it. This calcification process is influenced by aging, chronic inflammation, and long-term exposure to risk factors like high LDL/apB, high blood pressure, high blood sugar/insulin levels, and smoking.
How does plaque buildup in arteries?
Now that you know what causes plaque in arteries, it’s important to understand how it builds up. Plaque builds up when cholesterol-carrying particles, particularly apoB-containing ones, slip into a damaged artery lining, become oxidized, and trigger inflammation. Over time, immune cells, fats, and other materials accumulate in the artery wall and form plaque, which can grow and eventually calcify.
Where does plaque buildup in arteries?
Plaque buildup can occur in any artery in the body, but it most commonly affects the coronary (heart) arteries, carotid (brain), renal (kidneys), and femoral (legs) arteries. These are the arteries that supply major organs and are exposed to higher blood flow stress. Women are also more likely to develop microvascular disease, which affects the small arteries and can cause symptoms even when major arteries look clear.
What causes blockage in arteries?
A blockage in your arteries can happen when plaque builds up and eventually becomes large enough to narrow the space where blood flows. If a plaque ruptures, a blood clot can form on top of it and completely block the artery, or a piece of soft plaque can break off and travel downstream, blocking a smaller vessel. Either situation can lead to a heart attack, stroke, or another serious event.
When to See a Doctor or Registered Dietitian
If you’ve been told you have high cholesterol, high apoB, elevated lp(a), plaque, or an abnormal calcium score, it’s important to work with a healthcare provider who can guide you.
A doctor can diagnose conditions, order cardiac testing, monitor medications, and evaluate your symptoms.
A cardiovascular dietitian supports the day-to-day side of your care, interpreting labs, creating a personalized nutrition plan, and helping you make lifestyle changes that actually lower your risk.
If your numbers aren’t improving, you feel overwhelmed by conflicting advice, or you want a science-based approach designed specifically for you, this is exactly when 1:1 nutrition counseling can make the biggest difference in your heart health. Book a free discovery call today to get started.
References
- National Heart, Lung, and Blood Institute. (n.d.). Atherosclerosis. U.S. Department of Health and Human Services, National Institutes of Health.https://www.nhlbi.nih.gov/health/atherosclerosis
- Ogobuiro, I., Wehrle, C. J., & Tuma, F. (2023). Anatomy, thorax, heart coronary arteries. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK534790/
- Sethi, D., Gofur, E. M., & Munakomi, S. (2023). Anatomy, head and neck: Carotid arteries. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK545238/
- Leslie, S. W., & Sajjad, H. (2023). Anatomy, abdomen and pelvis: Renal artery. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459158/
- Swift, H., & Bordoni, B. (2023). Anatomy, bony pelvis and lower limb: Femoral artery. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK538262/
- Zemaitis, M. R., Boll, J. M., & Dreyer, M. A. (2023). Peripheral arterial disease. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK430745/
- Valdivielso, J. M., Rodríguez-Puyol, D., Pascual, J., Barrios, C., Bermúdez-López, M., Sánchez-Niño, M. D., Pérez-Fernández, M., & Ortiz, A. (2019). Atherosclerosis in chronic kidney disease: More, less, or just different? Arteriosclerosis, Thrombosis, and Vascular Biology, 39 (10), 1938–1946. https://www.ahajournals.org/doi/10.1161/ATVBAHA.119.312705
- Huang, Y. T., Hong, F. F., & Yang, S. L. (2021). Atherosclerosis: The Culprit and Co-victim of Vascular Dementia. Frontiers in neuroscience, 15, 673440. https://doi.org/10.3389/fnins.2021.673440
- Banerjee, C., & Chimowitz, M. I. (2017). Stroke caused by atherosclerosis of the major intracranial arteries. Circulation Research, 120(3), 502–513.
- https://www.ahajournals.org/doi/10.1161/circresaha.116.308441
- Carmena, R., Duriez, P., & Fruchart, J.-C. (2004). Atherogenic lipoprotein particles in atherosclerosis. Circulation, 109 (23_suppl_1), III-2–III-7.
- https://www.ahajournals.org/doi/10.1161/01.cir.0000131511.50734.44#sec-2
- Poznyak, A. V., Sadykhov, N. K., Kartuesov, A. G., Borisov, E. E., Melnichenko, A. A., Grechko, A. V., & Orekhov, A. N. (2022). Hypertension as a risk factor for atherosclerosis: Cardiovascular risk assessment. Frontiers in cardiovascular medicine, 9, 959285. https://doi.org/10.3389/fcvm.2022.959285
- Blaustein, J. R., Quisel, M. J., Hamburg, N. M., & Wittkopp, S. (2024). Environmental impacts on cardiovascular health and biology: An overview. Circulation Research, 134(9), 1048–1060. https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.123.323613
- Wei, T., Liu, J., Zhang, D., Wang, X., Li, G., Ma, R., Chen, G., Lin, X., & Guo, X. (2021). The Relationship Between Nutrition and Atherosclerosis. Frontiers in bioengineering and biotechnology, 9, 635504. https://doi.org/10.3389/fbioe.2021.635504
- Al-Mamari A. (2009). Atherosclerosis and physical activity. Oman medical journal, 24(3), 173–178. https://doi.org/10.5001/omj.2009.34
- Yao, B. C., Meng, L. B., Hao, M. L., Zhang, Y. M., Gong, T., & Guo, Z. G. (2019). Chronic stress: a critical risk factor for atherosclerosis. The Journal of international medical research, 47(4), 1429–1440. https://doi.org/10.1177/0300060519826820
- Libby, P., Ridker, P. M., & Maseri, A. (2002). Inflammation and atherosclerosis. Circulation, 105(9), 1135–1143.https://doi.org/10.1161/hc0902.104353
- Kovacic, S., & Bakran, M. (2012). Genetic susceptibility to atherosclerosis. Stroke research and treatment, 2012, 362941. https://doi.org/10.1155/2012/362941
- Poznyak, A., Grechko, A. V., Poggio, P., Myasoedova, V. A., Alfieri, V., & Orekhov, A. N. (2020). The Diabetes Mellitus-Atherosclerosis Connection: The Role of Lipid and Glucose Metabolism and Chronic Inflammation. International journal of molecular sciences, 21(5), 1835. https://doi.org/10.3390/ijms21051835
- Man, J. J., Beckman, J. A., & Jaffe, I. Z. (2020). Sex as a Biological Variable in Atherosclerosis. Circulation research, 126(9), 1297–1319. https://doi.org/10.1161/CIRCRESAHA.120.315930 https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.120.315930