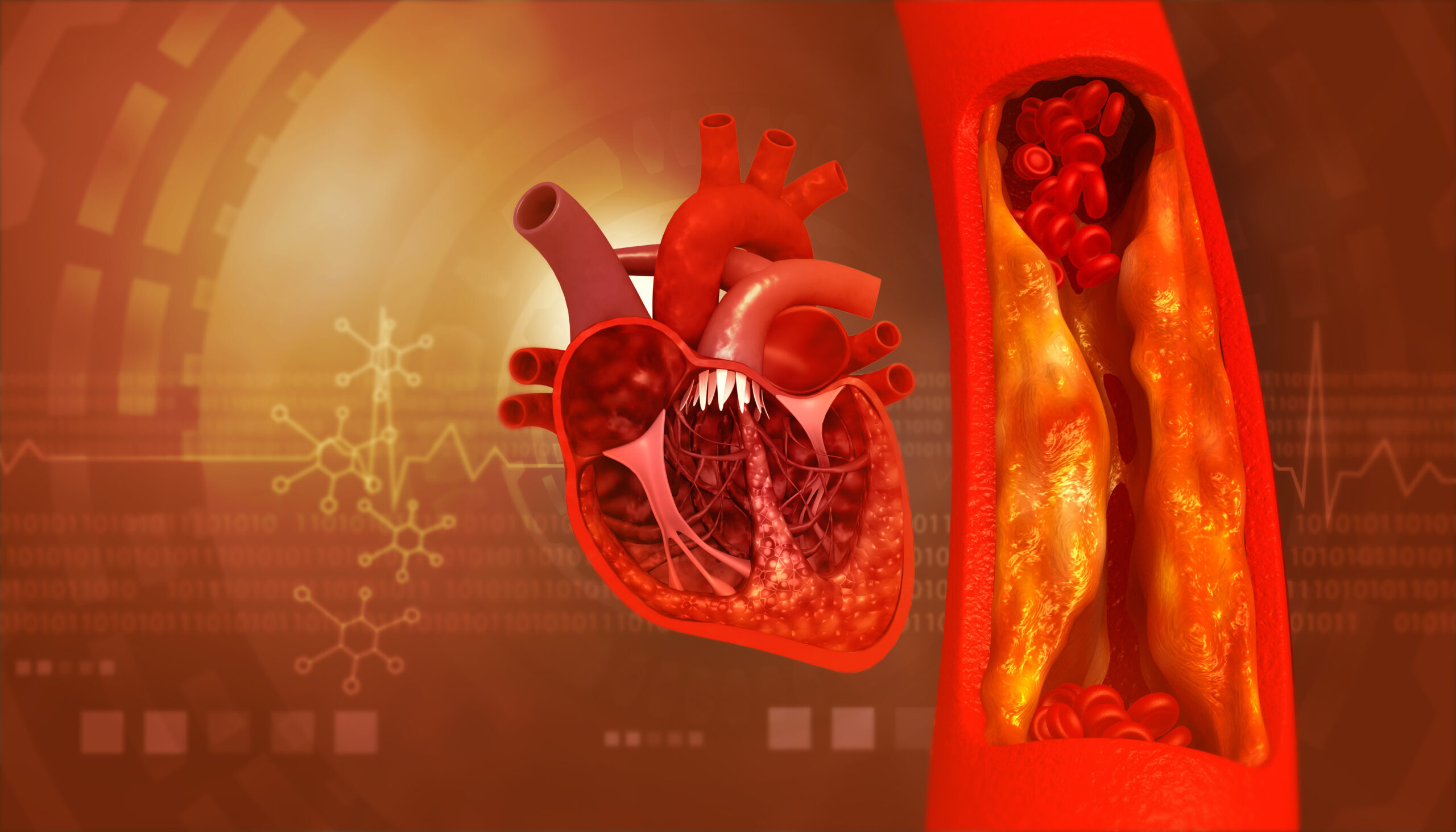
Your heart is the epicenter of your cardiovascular system, which is responsible for supplying oxygen and nutrients to various tissues and organs, including the heart itself. For this system to function at its best, it’s critical to have clear arteries. One of the best ways to ensure arterial health is to follow a nutrient-dense, heart-healthy diet — rich in vitamins that remove plaque from arteries.
What is Arterial Plaque?
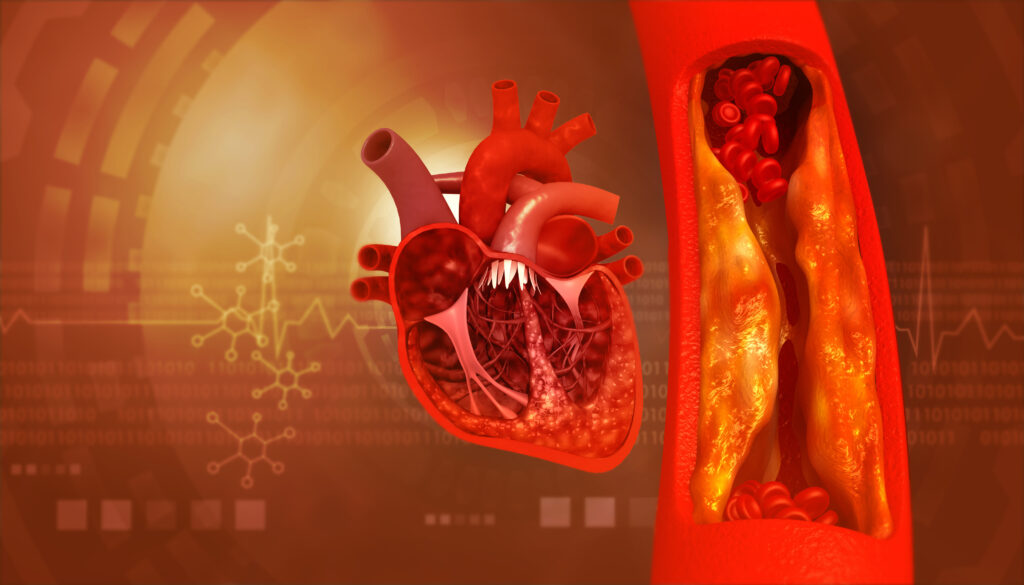
Arterial plaque refers to the accumulation of cholesterol, fat, calcium, cellular waste, and fibrin, on the inner walls of the arteries. A calcium-score heart scan can tell you whether you have calcium deposits, and other plaque buildup, present in your arteries.
When your arteries are clogged with plaque and other fatty deposits, this can lead to a progressive condition called atherosclerosis. Plaque buildup results in narrowed arteries and disruption of normal blood flow, increasing your risk for a heart attack.
Risk Factors
Many people have varying risk factors for heart disease that need to be addressed. Some of them can be more effectively managed than others. Consider which of your potential risk factors you can target through healthy lifestyle adjustments.
Risk factors you can change
- High Blood Pressure: This can damage the walls of arteries over time, making them more susceptible to plaque buildup.
- High LDL: Elevated levels of LDL “bad” cholesterol can lead to the deposition of cholesterol in arterial walls.
- Low HDL: HDL “good” cholesterol helps remove LDL from the bloodstream. Low levels of HDL are associated with an increased risk of atherosclerosis.
- Smoking: Smoking damages the endothelium, increases inflammation, and promotes the formation of arterial plaque. Additionally, it lowers HDL.
- Diabetes: Individuals with diabetes are at an increased risk of atherosclerosis. High blood sugar levels can damage blood vessels and contribute to plaque formation.
- Obesity: Excess body weight, particularly abdominal obesity, is associated with various risk factors for atherosclerosis, including high blood pressure, high cholesterol levels, and insulin resistance.
- Physical Inactivity: Lack of physical activity is a risk factor for atherosclerosis. Exercise helps maintain a healthy weight, lowers blood pressure, and improves cholesterol levels.
- Dietary Factors: Diets high in saturated and trans fats, cholesterol, and refined carbohydrates contribute to elevated cholesterol levels and can promote atherosclerosis.
- Insulin Resistance: Insulin resistance means the body becomes less responsive to insulin, which promotes high blood pressure, inflammation, and endothelial dysfunction.
- Oxidative Stress: Oxidative stress can lead to the inflammation and damage of blood vessel walls, initiating the cascade of events that result in atherosclerosis.
- Inflammatory Conditions: Chronic systemic inflammation can contribute to arterial plaque formation and its progression. While chronic inflammatory conditions, such as rheumatoid arthritis, psoriatic arthritis or lupus, can be genetic, when they are well managed they can potentially go into remission, and reduce their inflammatory toll on the body.
Risk factors you can’t change
- Age: The risk of atherosclerosis increases with age. As people get older, the likelihood of developing plaque buildup in arteries also increases.
- Genetics: A family history of early heart disease can contribute to an individual’s risk. Genetic factors may influence cholesterol levels and the overall susceptibility to atherosclerosis.
- Gender: Men generally have a higher risk of atherosclerosis than premenopausal women. However, a woman’s risk increases after menopause.
Atherosclerosis is serious. You can manage it, keep it from getting worse, and sometimes even reverse it by prioritizing your nutrition.
Let’s take a look at 5 vitamins that remove plaque from arteries. It’s best to prioritize getting nutrients from whole food sources before adding any potential heart health supplements.
1. Vitamin C: A Powerful Antioxidant
Vitamin C, also known as ascorbic acid, plays a crucial role in supporting heart health and may contribute to the prevention of atherosclerosis. As an antioxidant, vitamin C helps protect the arteries from oxidative stress, a key factor in the development of arterial plaque.
It also supports the flexibility and integrity of blood vessels, promoting healthy endothelial function. Furthermore, vitamin C supports the synthesis of collagen, a structural protein essential for the maintenance of arterial walls.
Adequate vitamin C levels are associated with a lower risk of cardiovascular diseases, including atherosclerosis.
Best sources: Citrus fruits, strawberries, bell peppers, leafy greens, tomatoes, and potatoes
2. Vitamin K: Regulating Calcium in Arteries
Vitamin K has two forms. K1 is primarily involved in blood clotting and K2 has gained attention for its potential role in promoting heart health, regulating calcium, and preventing atherosclerosis.
Vitamin K2 is believed to help direct calcium away from arteries and into the bones, preventing its accumulation in arterial walls. This matters because excess calcium in arteries can contribute to the development of arterial plaque.
Best sources: Fermented dairy products, certain cheeses, and natto (a traditional Japanese dish made from fermented soybeans)
3. Vitamin D: Supporting Heart Health
Vitamin D, often called the “sunshine vitamin,” has been recognized for its potential role in promoting heart health and reducing the risk of atherosclerosis.
Adequate vitamin D may help support healthy blood pressure, reduce arterial stiffness, and support immune function. It may also help maintain the integrity of blood vessel walls and inhibit processes that lead to plaque formation.
It’s important to get enough calcium along with your vitamin D intake, otherwise, it will begin leaching from your bones, leading to potential calcium vascularization. Calcium and vitamin D together are also an important combo for preventing osteoporosis.
Note that while calcium supplements are an option, doses above 500 mg per day can lead to calcium vascularization — so, prioritize getting calcium through food sources instead.
Best sources: Sun exposure, fatty fish, fortified foods, and vitamin D supplements (as directed by your healthcare provider)
4. Vitamin E: An Antioxidant for Arterial Health
Vitamin E is a fat-soluble antioxidant. It plays a significant role in supporting heart health and may have protective effects against atherosclerosis. As an antioxidant, vitamin E helps neutralize free radicals, molecules that can contribute to oxidative stress and inflammation.
Note that getting vitamin E through dietary sources is best. Some research has found that vitamin E taken in supplemental form can increase the risk of heart failure.
Best sources: Nuts, seeds, vegetable oils, and green leafy vegetables
5. Vitamin B3 (Niacin): Lowering Bad Cholesterol
Niacin (vitamin B3) offers potential benefits for heart health and addressing factors associated with atherosclerosis, like targeting abnormal lipid levels.
Doses of 1-3 grams per day may help lower levels of LDL cholesterol while increasing levels of HDL cholesterol. Some sources say using niacin can reduce LDL by up to 25% and raise HDL by up to 30%, which can sound intriguing.
However, note that the American Heart Association says there’s not enough evidence to recommend niacin supplements to lower cholesterol. For example, a 2017 Cochrane review found that niacin supplements didn’t reduce overall, heart-related, or non‐cardiovascular mortality or non-fatal heart attacks or strokes.
There is also a potential for liver damage when taking supplemental niacin, especially in high doses. Therefore, you should never just start a niacin supplement (or any heart health supplements) without being under the guidance of your healthcare provider and having your labs closely monitored.
Still, you can get niacin from foods in your diet and consider using a healthcare provider-recommended niacin supplement in conjunction with other cholesterol-lowering approaches.
Best sources: Fish, poultry, beef, pork, peanuts, whole grains, seeds, mushrooms, leafy greens, dairy products, and fortified foods
Lifestyle and Dietary Considerations
One of the best things you can do for your heart — and overall health — is to eat a nutrient-dense diet and practice healthy lifestyle habits. Consider the following:
- Nutrition: A heart-healthy diet emphasizes minimally processed foods like fruits, vegetables, legumes, nuts, seeds, lean proteins, and healthy fats. This kind of diet needs to be rich in the vitamins that remove plaque from arteries we discussed above. Avoid ultra-processed foods that are high in added sugar, saturated fat, and sodium.
- Exercise: A heart-healthy lifestyle includes regular exercise. Aim for at least 30-60 minutes of intentional movement most days. Include a variety of aerobic exercises and resistance training.
- Stress management: Chronic stress promotes systemic inflammation, disrupts blood sugar regulation, elevates blood pressure, and heightens levels of the stress hormones cortisol and adrenaline, all of which can damage the heart.
If you’re interested in learning more about how science-based nutrition can work for your heart, join my next 6 week heart optimization group program or schedule a 1:1 discovery call with me for personalized guidance. We will discuss diet, lifestyle, heart health supplements, and more for optimal heart health and longevity.
References
1. Libby P, Buring JE, Badimon L, et al. Atherosclerosis. Nat Rev Dis Primers. 2019;5(1):56. Published 2019 Aug 16. doi:10.1038/s41572-019-0106-z
2. Pahwa R, Jialal I. Atherosclerosis. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507799/
3. Moser MA, Chun OK. Vitamin C and Heart Health: A Review Based on Findings from Epidemiologic Studies. Int J Mol Sci. 2016;17(8):1328. Published 2016 Aug 12. doi:10.3390/ijms17081328
4. Ivanov V, Ivanova S, Niedzwiecki A, Rath M. Vitamin C inhibits the calcification process in human vascular smooth muscle cells. Am J Cardiovasc Dis. 2020;10(2):108-116. Published 2020 Jun 15.
5. Bellinge JW, Dalgaard F, Murray K, et al. Vitamin K Intake and Atherosclerotic Cardiovascular Disease in the Danish Diet Cancer and Health Study. J Am Heart Assoc. 2021;10(16):e020551. doi:10.1161/JAHA.120.020551
6. Hariri E, Kassis N, Iskandar JP, et al. Vitamin K2-a neglected player in cardiovascular health: a narrative review. Open Heart. 2021;8(2):e001715. doi:10.1136/openhrt-2021-001715
7. Carbone F, Liberale L, Libby P, Montecucco F. Vitamin D in atherosclerosis and cardiovascular events. Eur Heart J. 2023;44(23):2078-2094. doi:10.1093/eurheartj/ehad165
8. Voulgaridou G, Papadopoulou SK, Detopoulou P, et al. Vitamin D and Calcium in Osteoporosis, and the Role of Bone Turnover Markers: A Narrative Review of Recent Data from RCTs. Diseases. 2023;11(1):29. Published 2023 Feb 8. doi:10.3390/diseases11010029
9. Garg A, Lee JC. Vitamin E: Where Are We Now in Vascular Diseases?. Life (Basel). 2022;12(2):310. Published 2022 Feb 18. doi:10.3390/life12020310
10. Shah S, Shiekh Y, Lawrence JA, et al. A Systematic Review of Effects of Vitamin E on the Cardiovascular System. Cureus. 2021;13(6):e15616. Published 2021 Jun 12. doi:10.7759/cureus.15616
11. D’Andrea E, Hey SP, Ramirez CL, Kesselheim AS. Assessment of the Role of Niacin in Managing Cardiovascular Disease Outcomes: A Systematic Review and Meta-analysis. JAMA Netw Open. 2019;2(4):e192224. Published 2019 Apr 5. doi:10.1001/jamanetworkopen.2019.2224
12. Djadjo S, Bajaj T. Niacin. [Updated 2023 Mar 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541036/
13. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Niacin. [Updated 2020 Jul 9]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548176/