Peripheral artery disease (PAD) is a common circulatory problem that puts you at an increased risk of severe cardiovascular events. Managing PAD requires more than medical interventions. It’s important to make changes to your lifestyle to improve symptoms and support overall vascular health.
What is Peripheral Artery Disease (PAD)?
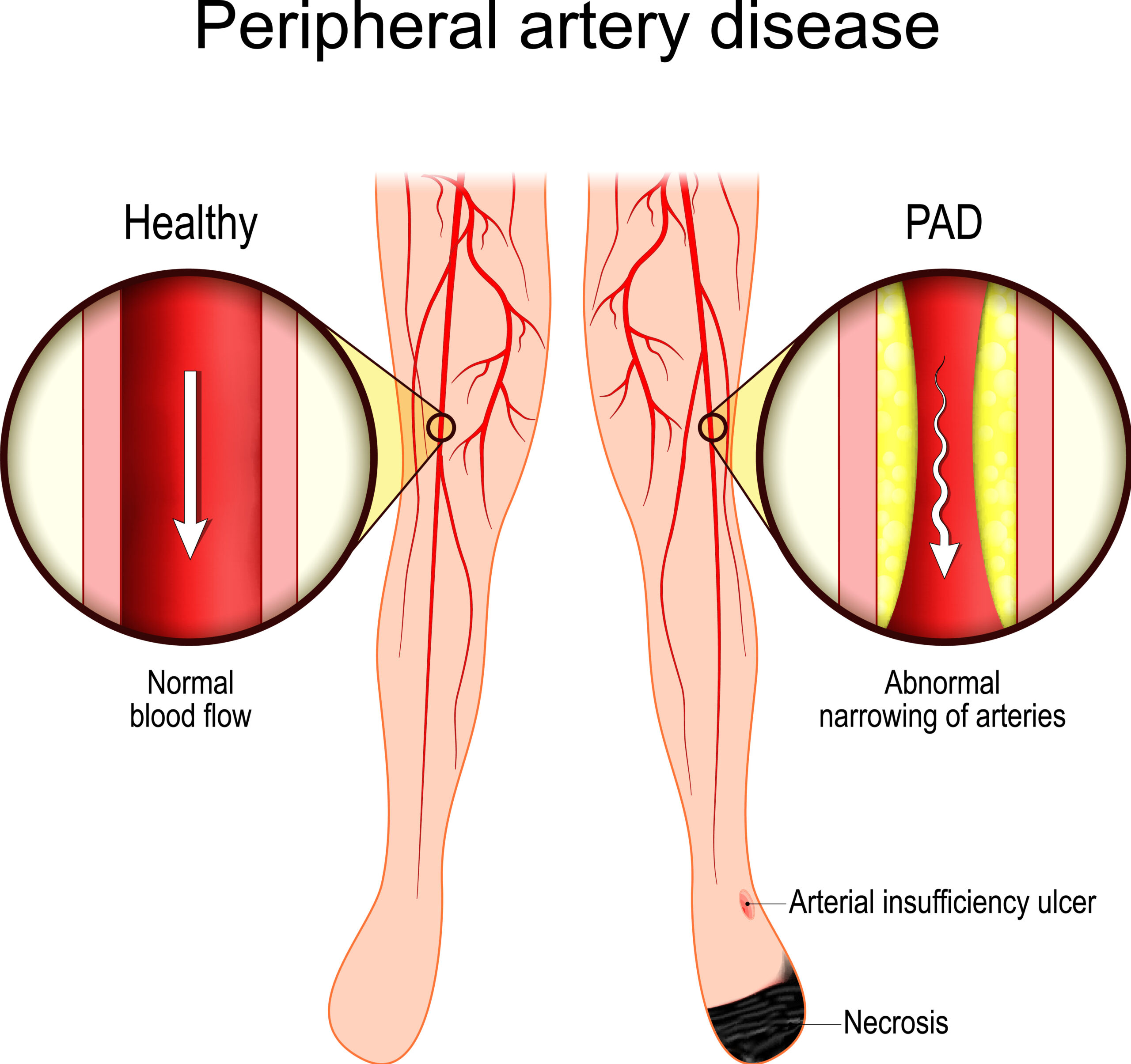
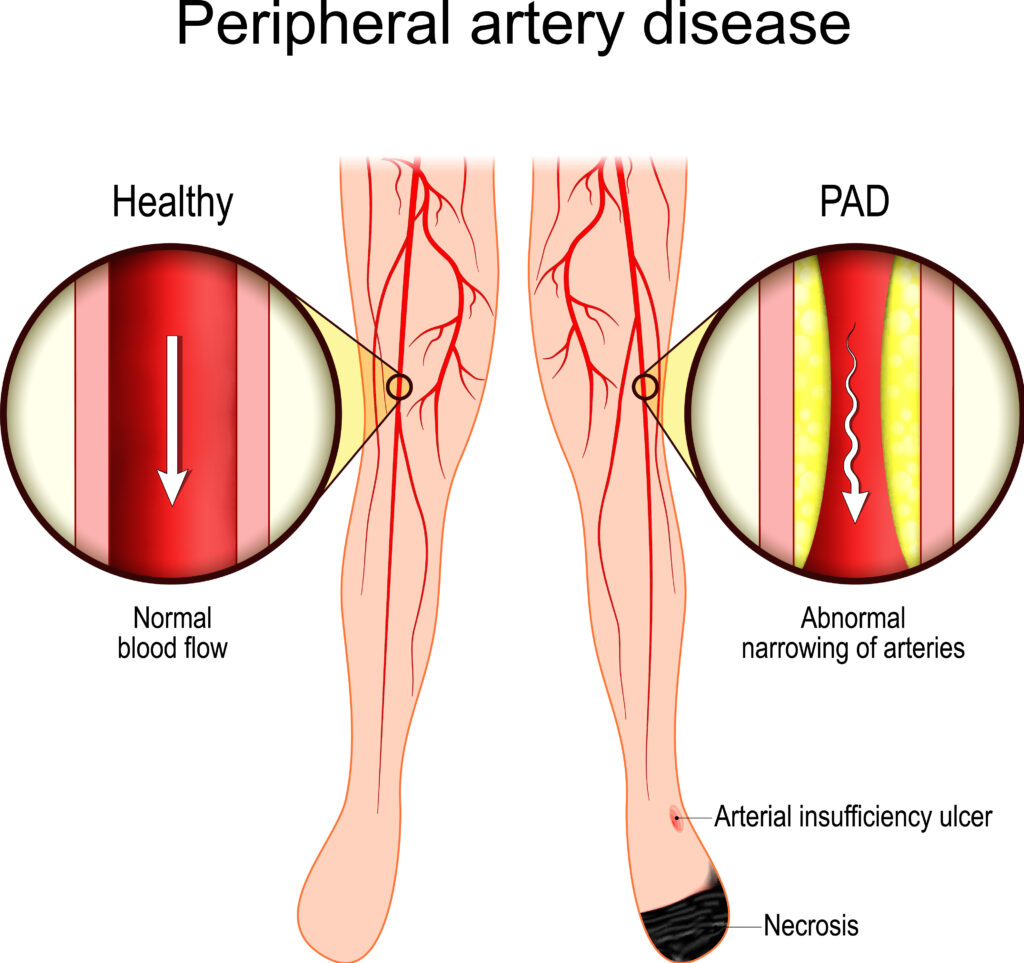
PAD is a vascular disease caused by plaque formation in the arteries that leads to narrowing and potential blockage of the arteries, particularly those running through the abdominal aorta, iliac, and lower extremities. When the lower extremity arteries are narrowed due to having too much artery-clogging cholesterol in the blood vessels, it can lead to leg pain called claudication.
When diagnosing PAD your doctor may use several methods, including a physical exam to check for a weak pulse in your legs and an ultrasound or angiography to examine blood flow through your arteries. They may use the Ankle-Brachial Index (ABI) to compare the blood pressure in your ankle to that in your arm, which is a non-invasive procedure.
Unfortunately, PAD is underdiagnosed and undertreated — a big disservice to preventive heart attack risk reduction.
If PAD is suspected, blood tests for cholesterol, triglycerides, and blood sugar might be ordered to get a better picture of your overall cardiovascular health. This additional insight is warranted and important because of the underlying atherosclerotic cause of PAD. Plus, knowing your calcium artery score is a good idea as a high score may indicate an increased risk of PAD.
Lifestyle changes are extremely important for managing PAD, such as stopping smoking, exercising regularly, eating a nutrient-dense diet, and maintaining a healthy weight. Research suggests that adhering to a healthy diet pattern is an important factor in reducing the risk of men and women developing PAD in the first place, which we’ll focus on in this article.
If PAD isn’t properly managed, complications are likely. For example, you could develop critical limb ischemia, in which you have significantly reduced blood flow to your limbs that leads to pain, sores, or in some cases, gangrene, the death of tissue due to a lack of blood flow or a severe bacterial infection that may require limb amputation.
Untreated PAD also increases your risk of heart attacks and strokes due to the narrowing and hardening of your arteries, reduced blood flow, inflammation, and increased clotting risk.
Individuals with high blood pressure have a 2.5 to 4x increased risk of PAD, and those with high cholesterol have a 2x increased risk. Smoking can increase the risk of PAD by 4 times. And 42% of individuals who have coronary artery disease also have PAD.
The good news is that we can prevent PAD by managing these conditions that increase your risk for PAD through science-based nutrition.
PAD versus PVD
You may have heard of PVD, but what’s the difference between peripheral vascular disease vs peripheral arterial disease? PAD specifically refers to what’s happening with circulation and your limbs.
PVD is a broader term that includes PAD plus any disorder affecting the blood vessels outside your heart and brain. For instance, PVD may refer to conditions like deep vein thrombosis and chronic venous insufficiency.
Diet for Peripheral Artery Disease
A heart-healthy diet supports your overall vascular health and helps manage PAD. When you have endothelial dysfunction and atherosclerosis, optimal nutrition can address the pro-oxidative and inflammatory state of your body, improve PAD symptoms, and help prevent its progression.
Furthermore, studies have found that PAD patients eat fewer vegetables and get less fiber, vitamins C and E, folate, and long-chain polyunsaturated fatty acids than people without PAD.
I recommend an anti-inflammatory diet to my clients, emphasizing nutrients found in the Dietary Inflammatory Index (DII) to lower inflammation. The DII is a tool used to assess the inflammatory potential of a person’s diet based on their intake of various food components that have been shown to either increase or decrease inflammation. An anti-inflammatory diet is also naturally going to be higher in the nutrients people with PAD may be lacking.
Another tool used by some researchers is called the Anti-inflammatory Diet Index (AIDI), which was created to predict low-grade systemic chronic inflammation. A higher AIDI is associated with a higher degree of inflammation as well as an increased risk of heart failure, abdominal aortic aneurysm, venous thromboembolism, and cardiovascular-related death.
In one study, researchers evaluated the associations of individual food groups in the AIDI with PAD risk. They found that eating a lot of breakfast cereals, chocolate, and red wine, as well as the use of olive/canola oil, was associated with a lower risk of PAD and that high consumption of processed red meat and organ meats was associated with a higher risk of PAD.
Along the same lines, evidence shows eating a pro-inflammatory diet is associated with a higher risk of PAD. In another study, researchers obtained the dietary inflammatory index of foods using a 24-hour recall among participants, which included 5840 individuals from the 1999–2004 National Health and Nutrition Examination Survey (NHANES). They consistently found a positive association between a pro-inflammatory eating pattern and the risk of PAD.
Taking all of this into consideration when designing a peripheral artery disease diet, let’s talk about foods to avoid with PAD and what to eat more often to protect yourself.
Foods to include for PAD
Research has shown that a Mediterranean-style diet pattern — which is plant-forward with an emphasis on unsaturated fats, fiber, and lean proteins — is associated with a lower incidence of PAD. Based on this, below are some of the best foods to eat regularly, as they’re nutrient-rich and anti-inflammatory.
- Fiber-rich carbohydrates: Fiber is only found in plants. It helps lower LDL cholesterol levels by binding to cholesterol and getting rid of it. Additionally, fiber-rich diets improve blood sugar control and support weight management, both of which are crucial for reducing the risk of heart disease. Consume plenty of fruits, vegetables, whole grains, and legumes to optimize your fiber intake and vascular health.
- Healthy fats: Opt for sources of unsaturated fats such as olive oil, nuts, seeds, and fatty fish rich in omega-3 fatty acids to help reduce inflammation and improve blood lipid profiles. These fats should replace saturated and trans fats found in red meat, full-fat dairy products, and fast food items that promote higher LDL levels and plaque buildup in the arteries.
- Antioxidant-rich foods: Add more colorful berries, leafy greens, cruciferous vegetables, and tomatoes to help fight oxidative stress and support overall vascular health.
- Lean proteins: Lean proteins like fish, poultry, legumes, and soy foods are low in saturated fat and better for vascular health.
Foods to avoid with PAD
As you increase your intake of foods that provide essential nutrients, these can replace some less healthy foods you might be eating. Consider where some of these nutrients can be reduced in your diet:
- Saturated and trans fats: Found in large amounts in meat, full-fat dairy, coconut, palm oil, and fast food items, and can negatively impact your cholesterol and arterial health.
- Excessive sodium: Eating a lot of added salt is associated with hypertension and an increased risk for PAD. Cut down on salt added when cooking and avoid packaged convenience foods.
- Sugary foods and beverages: Added sugar is everywhere, including packaged snack foods, breakfast cereals, snack bars, and drinks like soda, energy drinks, and fruit juices. Excessive sugar consumption is associated with a higher risk for diabetes, obesity, and cardiovascular complications like PAD.
Exercise and Physical Activity for PAD
Regular physical activity is important for improving circulation and managing PAD. Moving your body helps promote the development of new blood vessels, enhance blood flow to your limbs, and reduce arterial stiffness.
The best exercises for peripheral artery disease are ones you can do regularly, particularly lower-impact options. Consider walking, swimming, biking, dancing, aerobics, strength training, and yoga, and avoid staying sedentary for long periods. These movements can alleviate PAD symptoms like leg pain and cramps. Regular stretching is also important for PAD as it helps reduce arterial stiffness, improve blood flow, enhance flexibility, and reduce pain and discomfort in the affected limbs.
Plus, regular exercise is crucial for overall cardiovascular health, as it strengthens the heart muscle, improves its efficiency in pumping blood throughout the body, and enhances the function of blood vessels. Moving your body helps to lower blood pressure, reduce LDL cholesterol, increase HDL cholesterol, and improve overall circulation, reducing the risk of heart disease and stroke. Plus, exercise supports healthier weight management and reduces stress.
Client Success Story
A 55-year-old woman consulted me because she was struggling with peripheral artery disease (PAD) and was confused about what to eat. She had constant pains in her legs and difficulty walking short distances, which diminished her quality of life.
She had a significant family history of heart disease and her medical history showed elevated blood pressure (130/80 mmHg), a waist circumference of 39 inches, high blood sugar levels (103 mg/dL, no HgA1c tested), and high cholesterol (LDL 130 mg/dL). She started to notice these trends during menopause, and her doctor was not overtly concerned.
When she started having pains in her legs, she was prescribed medications but it didn’t provide relief.
We worked together and focused on implementing an anti-inflammatory, nutrient-sufficient diet. Prior, she had cut out all “the bad” foods but did not focus on adding in the heart healthy foods that help with improving her blood vessel health.
After implementing science based nutrition, in 3 weeks, her BP optimized to 112/72mmHg and she noticed a reduction in the inflammation in her legs. She mentioned how the constant throbbing and aching began to subside, and she felt she was able to move more freely without discomfort.
After a month and a half, improvements continued, and her energy levels increased and it allowed her to incorporate more exercises into her routine with ease.
Six months later, her waist circumference decreased to 34 inches, blood sugar normalized to 93 mg/dL with an HgA1c of 5.4% (normal <5.7%), and cholesterol levels dropped by 48 points to 82 mg/dL.
She kept going to her regular doctor appointments and it showed a noticeable improvement in the circulation in her legs. Her energy levels continued to stay high and she managed her condition well.
It was a testament to the power of nutrition in healing the body from within.
PAD and Lifestyle: Takeaway
PAD is a serious condition that requires meaningful lifestyle changes to improve and prevent it from worsening. A diet that prioritizes fiber, vitamins, minerals, antioxidants, and omega-3s, while avoiding excessive sodium, saturated fat, and added sugar, along with regular exercise, can make a significant difference in improving circulation and cardiovascular health.
When someone faces a new diagnosis, having personalized guidance from a Registered Dietitian who specializes in their medical conditions helps them make remarkable changes. If you need support on your heart health journey, I would be happy to help you. Click here to learn more about my 1:1 services or consider my 6 week group Heart Health Optimization program.
References
- Chen GC, et al. Adherence to Recommended Eating Patterns Is Associated With Lower Risk of Peripheral Arterial Disease: Results From the Women’s Health Initiative. Hypertension. 2021;78:447–455.
- Yuan S, Bruzelius M, Damrauer SM, et al. Anti-inflammatory diet and incident peripheral artery disease: Two prospective cohort studies. Clin Nutr. 2022;41(6):1191-1196. doi:10.1016/j.clnu.2022.04.002
- Elfghi, M., Jordan, F., Dunne, D. et al. The effect of lifestyle and risk factor modification on occlusive peripheral arterial disease outcomes: standard healthcare vs structured programme—for a randomised controlled trial protocol. Trials 22, 138 (2021). https://doi.org/10.1186/s13063-021-05087-x
- Soyoye DO, Abiodun OO, Ikem RT, Kolawole BA, Akintomide AO. Diabetes and peripheral artery disease: A review. World J Diabetes. 2021;12(6):827-838. doi:10.4239/wjd.v12.i6.827
- Delaney CL, Smale MK, Miller MD. Nutritional Considerations for Peripheral Arterial Disease: A Narrative Review. Nutrients. 2019;11(6):1219. Published 2019 May 29. doi:10.3390/nu11061219
- Nosova EV, Conte MS, Grenon SM. Advancing beyond the “heart-healthy diet” for peripheral arterial disease. J Vasc Surg. 2015;61(1):265-274. doi:10.1016/j.jvs.2014.10.022
- Fan H, et al. A Proinflammatory Diet Is Associated with Higher Risk of Peripheral Artery Disease. Nutrients 2022, 14(17), 3490.
- Adegbola A, Behrendt CA, Zyriax BC, Windler E, Kreutzburg T. The impact of nutrition on the development and progression of peripheral artery disease: A systematic review. Clin Nutr. 2022;41(1):49-70. doi:10.1016/j.clnu.2021.11.005
- Soliman GA. Dietary Fiber, Atherosclerosis, and Cardiovascular Disease. Nutrients. 2019;11(5):1155. Published 2019 May 23. doi:10.3390/nu11051155
- Wierenga KA, Pestka JJ. Omega-3 Fatty Acids And Inflammation – You Are What You Eat!. Front Young Minds. 2021;9:601068. doi:10.3389/frym.2021.601068
- Keramat S, Sharebiani H, Patel M, Fazeli B, Stanek A. The Potential Role of Antioxidants in the Treatment of Peripheral Arterial Disease: A Systematic Review. Antioxidants (Basel). 2022;11(11):2126. Published 2022 Oct 28. doi:10.3390/antiox11112126
- Diab A, Dastmalchi LN, Gulati M, Michos ED. A Heart-Healthy Diet for Cardiovascular Disease Prevention: Where Are We Now?. Vasc Health Risk Manag. 2023;19:237-253. Published 2023 Apr 21. doi:10.2147/VHRM.S379874
- Grillo A, Salvi L, Coruzzi P, Salvi P, Parati G. Sodium Intake and Hypertension. Nutrients. 2019;11(9):1970. Published 2019 Aug 21. doi:10.3390/nu11091970
- Kato M, Nihei Green F, Hotta K, et al. The Efficacy of Stretching Exercises on Arterial Stiffness in Middle-Aged and Older Adults: A Meta-Analysis of Randomized and Non-Randomized Controlled Trials. Int J Environ Res Public Health. 2020;17(16):5643. Published 2020 Aug 5. doi:10.3390/ijerph17165643