We most often hear about calcium in terms of how it supports bone health, but did you know it’s also important for your heart? In this blog, I’m digging into the relationship between calcium and heart disease. I want to clear any misconceptions about coronary artery calcium score and how to optimize calcium from your diet.
The Role of Calcium in Heart Health
Your heart is a muscle that needs calcium to contract and relax. Calcium is also essential for your heart’s electrical conduction system to work properly, which regulates your heartbeat.
Having enough calcium in your body supports the strength and integrity of the heart so it can efficiently pump blood throughout your body. Plus, calcium is involved in blood pressure regulation by influencing the contraction and dilation of blood vessels.
Imbalances in your calcium levels can potentially increase your risk of cardiovascular diseases including hypertension and arrhythmias.
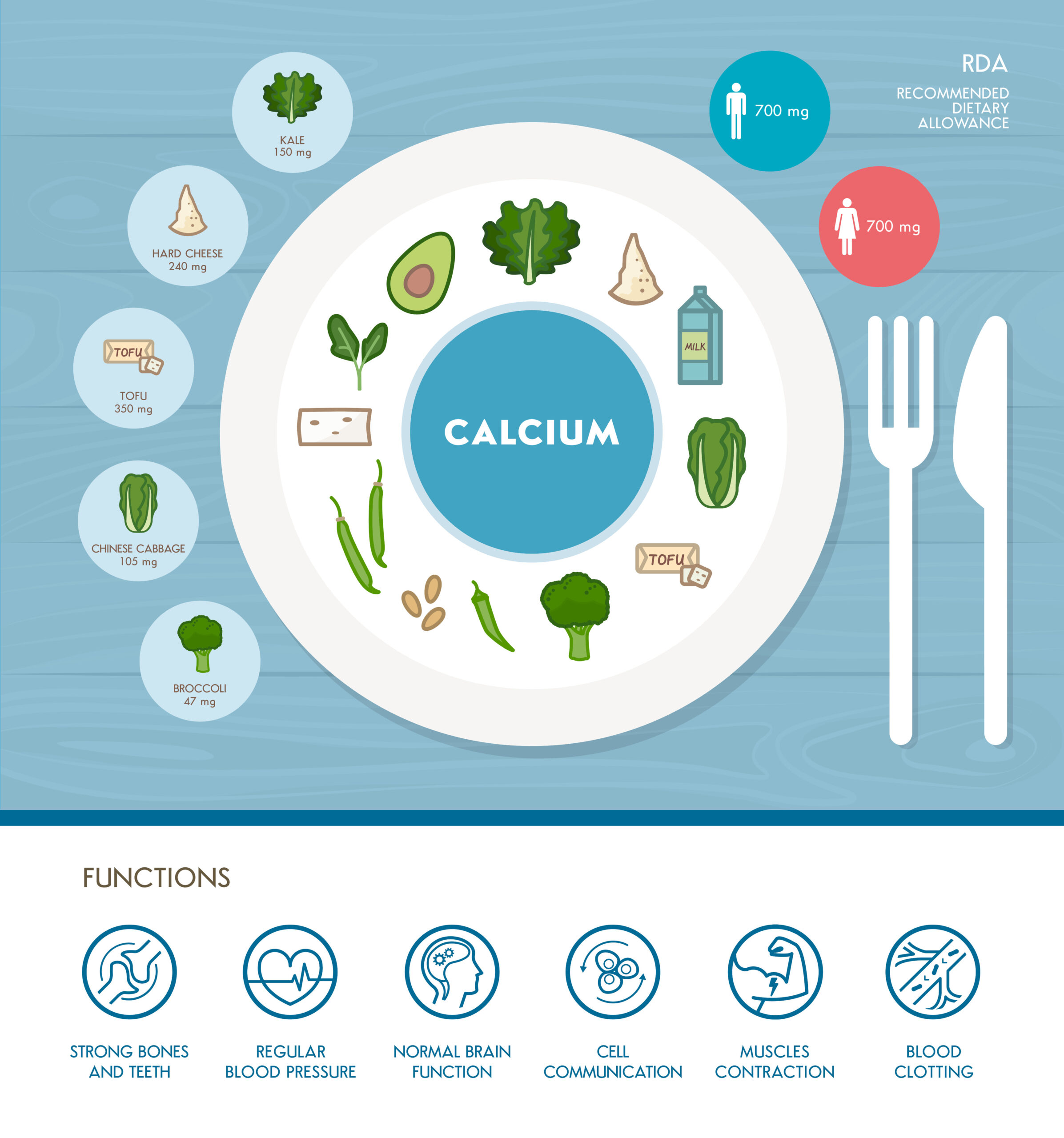
Needless to say, it’s important to ensure you’re getting enough calcium. Daily calcium needs vary depending on factors such as age, gender, pregnancy status, and individual health conditions. However, most adults should get 1000-1200 milligrams per day.
Foods High in Calcium
First and foremost, I recommend aiming to meet your calcium needs through food. There are plenty of calcium-rich foods to choose from, such as:
- Dairy, such as cow’s milk, yogurt, and cheese
- Leafy greens, like kale, spinach, collard greens, and bok choy
- Fortified foods, including certain cereals, orange juices, breads, and plant-based milk
- Canned fish with bones, like sardines, salmon, and anchovies
- Nuts and seeds, especially almonds, chia seeds, and sesame seeds
- Legumes, like edamame, calcium-set tofu, and white beans
Many of these are foods high in calcium and vitamin D as well, which are both important for your heart.
How to Get Calcium Without Dairy
If you have a dairy allergy, are lactose intolerant, or avoid dairy for any reason, you can find calcium in leafy greens, canned fish with bones, nuts, seeds, legumes, and fortified foods.
However, certain plant-based calcium foods also contain high amounts of oxalates, compounds that can interfere with calcium absorption. Oxalates can bind to calcium and form oxalate crystals, which could potentially lead to kidney stones in susceptible individuals.
Some foods that have both calcium and oxalates include:
- Spinach
- Swiss chard
- Beet greens
- Rhubarb
- Almonds
- Cashews
- Sesame seeds
- Brazil nuts
- Peanut butter
- Cocoa powder
This doesn’t mean you shouldn’t eat these sources but reiterates the importance of eating a variety of calcium-containing foods to ensure you’re getting enough.
Calcium and Heart Disease Research
Research shows that a very high calcium intake, especially in supplemental form, is associated with a higher risk of cardiovascular disease. In one meta-analysis, calcium supplements increased this risk by 15% among healthy postmenopausal women. Again, this is why I recommend foods first.
Calcium Supplements and Heart Disease
Calcium supplements are widely used, especially among aging individuals to help prevent osteoporosis. However, while calcium supplements can have a place, they should be used with caution and only when recommended by a healthcare provider.
Two of the most commonly used calcium supplements are calcium citrate and calcium carbonate (Tums). Both can increase calcium intake, but they have some differences.
- Calcium carbonate is widely available and inexpensive. It contains the highest concentration of elemental calcium, so a smaller pill can provide a higher dose. It requires stomach acid for absorption, so it’s best taken with food.
- Calcium citrate is absorbed well even in the absence of stomach acid, making it a good option for individuals with low stomach acid production or who take antacids. It contains less elemental calcium per pill, so larger or more frequent doses may be required to achieve the same calcium intake as calcium carbonate.
If calcium supplements are necessary, don’t exceed 500mg in a sitting as this can promote calcification. Not getting enough calcium can also lead to calcification because the parathyroid hormone will begin to pull it from your bones. It’s a delicate balance and you should aim to meet your calcium needs with food.
Coronary Artery Calcium Score
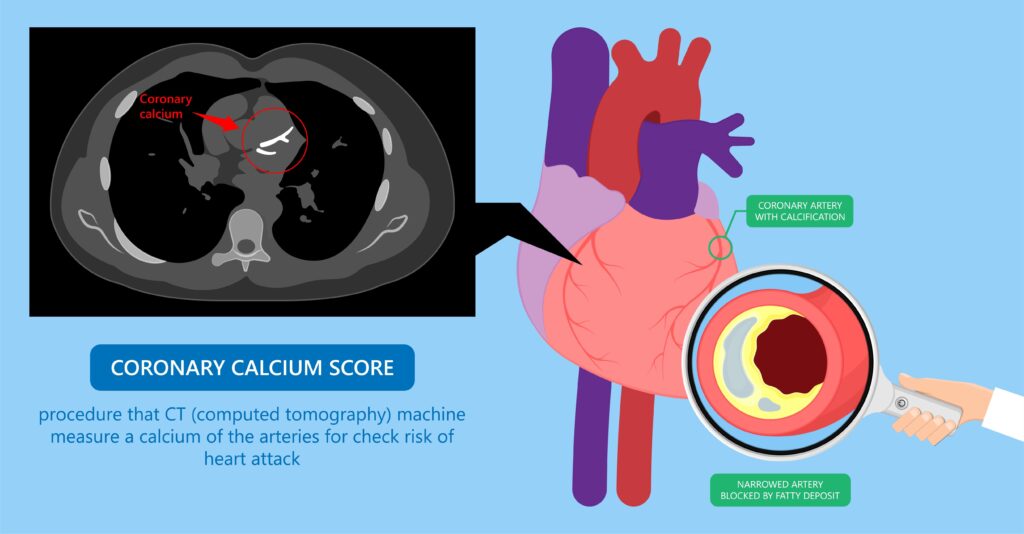
The coronary artery calcium score, or CAC, is used to assess the amount of calcium buildup in the walls of the coronary arteries, the blood vessels that supply your heart with oxygen-rich blood. It’s typically done using a non-invasive CT scan.
During the CT, high-resolution images of the heart are captured, allowing doctors to identify and evaluate any calcium deposits (plaques) building up in the coronary arteries. The CAC is calculated based on the calcifications present.
The CAC score indicates your risk of developing coronary artery disease or experiencing a heart attack. Higher calcium scores suggest more severe coronary artery calcification and a higher risk.
If you have a high CAC score, you might be wondering whether you should avoid calcium in your diet. The short answer is no, and I’ll explain it with osteoporosis.
Osteoporosis and Calcification
When someone has osteopenia or osteoporosis and isn’t getting enough calcium in their diet (and therefore not enough calcium in the blood), calcium is pulled from the bones and enters the vascular system. This can lead to calcium buildup in the arteries.
This demonstrates how important it is to make sure you’re getting enough calcium from your diet. A lack of calcium results in it being pulled from your bones in an attempt to balance what’s lacking. This ultimately sets you up for a higher risk of having more calcified plaque. So avoiding calcium when you have a high CAC, is going to make the situation worse, not better.
Client Success Story
A 64-year-old woman came to see me because she had osteoporosis and a high calcium score. She wasn’t sure how to get enough calcium without increasing her CAC.
She also had a weight loss goal, but this was likely stubborn due to insulin resistance (she had a HgA1c of 5.7%). Her cholesterol wasn’t optimized because of her diet. Her overall nutrient intake could have been improved for optimal bone mineral density.
We worked together in my VIP Intensive Program over 3 months where we addressed her insulin resistance, bowel health, and bone/heart health through a nutrient-sufficient diet.
In one month, she lost 2.5 inches off her waist and 4.6 pounds. In 3 months, she achieved her goal weight, had more energy, and felt good. Her labs and waist circumference were optimal at 6 months.
Lifestyle Factors Affecting Calcium Absorption and Heart Health
A Nutritional Matrix
In addition to knowing where you’re getting calcium from in your diet, there are a few other nutrients that work with calcium to support heart (and bone) health:
- Vitamin D: Plays a crucial role in regulating blood pressure, supporting endothelial function, and reducing inflammation.
- Magnesium: Helps regulate heart rhythm, maintain proper muscle function, and support the dilation of blood vessels, which supports healthy blood pressure levels.
- Vitamin K: Aids in the regulation of calcium deposition in the arteries, which helps prevent arterial calcification and maintains vascular elasticity.
These nutrients have to be in the proper matrix, which you can achieve through whole foods. This is why I’m a food-first practitioner. I help my clients optimize their diets through science-based nutrition and only recommend supplements on an individual basis when necessary and appropriate.
Exercise
Another important factor in bone health and optimal cardiovascular function is exercise. Studies show that resistance exercises, like strength training with dumbbells, weight machines, resistance bands, or bodyweight exercises, are particularly beneficial for bone density and lowering the risk of heart disease.
One study found that even less than one hour per week of resistance exercise, independent of aerobic exercise, is associated with a lower risk of cardiovascular disease and all-cause mortality. Exercise needs to also be coupled with nutrition to avoid oxidative stress which can increase your risk of plaque formation in the arteries.
Calcium and Your Heart: Final Thoughts
Getting enough calcium is essential for your overall wellness and supporting your heart. To reduce your risk of calcification and increased heart disease risk, it’s important to ensure you’re getting enough calcium without going overboard. The best way to do this is to eat a variety of calcium-rich foods in sufficient quantities and only utilize supplements if necessary and indicated by your healthcare team.
Looking for guidance to optimize your heart health through science based nutrition? Click here to learn about 1:1 counseling or consider joining my 6 week heart optimization group program.
References
- Calcium Fact Sheet for Health Professionals. Office of Dietary Supplements. Updated 3 Jan 2024. Available from: https://ods.od.nih.gov/factsheets/calcium-HealthProfessional/
- Bargagli M, Tio MC, Waikar SS, Ferraro PM. Dietary Oxalate Intake and Kidney Outcomes. Nutrients. 2020;12(9):2673. Published 2020 Sep 2. doi:10.3390/nu12092673
- Tankeu AT, Ndip Agbor V, Noubiap JJ. Calcium supplementation and cardiovascular risk: A rising concern. J Clin Hypertens (Greenwich). 2017;19(6):640-646. doi:10.1111/jch.13010
- Bolland MJ, Avenell A, Baron JA, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ. 2010;341:c3691. Published 2010 Jul 29. doi:10.1136/bmj.c3691
- Myung SK, Kim HB, Lee YJ, Choi YJ, Oh SW. Calcium Supplements and Risk of Cardiovascular Disease: A Meta-Analysis of Clinical Trials. Nutrients. 2021;13(2):368. Published 2021 Jan 26. doi:10.3390/nu13020368
- Yang C, Shi X, Xia H, et al. The Evidence and Controversy Between Dietary Calcium Intake and Calcium Supplementation and the Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Cohort Studies and Randomized Controlled Trials. J Am Coll Nutr. 2020;39(4):352-370. doi:10.1080/07315724.2019.1649219
- Reid IR, Birstow SM, Bolland MJ. Calcium and Cardiovascular Disease. Endocrinol Metab (Seoul). 2017;32(3):339-349. doi:10.3803/EnM.2017.32.3.339
- Czaja-Ziółkowska MZ, Wasilewski J, Gąsior M, Głowacki J. An update on the coronary calcium score: a review for clinicians. Postepy Kardiol Interwencyjnej. 2022;18(3):201-205. doi:10.5114/aic.2022.121035
- Martini N, Streckwall L, McCarthy AD. Osteoporosis and vascular calcifications. Endocr Connect. 2023;12(11):e230305. Published 2023 Oct 5. doi:10.1530/EC-23-0305
- de la Guía-Galipienso F, Martínez-Ferran M, Vallecillo N, Lavie CJ, Sanchis-Gomar F, Pareja-Galeano H. Vitamin D and cardiovascular health. Clin Nutr. 2021;40(5):2946-2957. doi:10.1016/j.clnu.2020.12.025
- DiNicolantonio JJ, Liu J, O’Keefe JH. Magnesium for the prevention and treatment of cardiovascular disease. Open Heart. 2018;5(2):e000775. Published 2018 Jul 1. doi:10.1136/openhrt-2018-000775
- Khalil Z, Alam B, Akbari AR, Sharma H. The Medical Benefits of Vitamin K2 on Calcium-Related Disorders. Nutrients. 2021;13(2):691. Published 2021 Feb 21. doi:10.3390/nu13020691
- Liu Y, Lee DC, Li Y, et al. Associations of Resistance Exercise with Cardiovascular Disease Morbidity and Mortality. Med Sci Sports Exerc. 2019;51(3):499-508. doi:10.1249/MSS.0000000000001822