Getting a variety of nutrients in your diet is important for overall health, but certain ones, like potassium, are especially involved in cardiovascular wellness. Getting too little or too much potassium can both have negative effects, so the best way to safely meet your needs is with a nutrient-sufficient, balanced diet.
Here’s what to know about potassium and the heart, including what food has potassium and the relationship between potassium and heart failure.
The Science of Potassium and Heart Health
Potassium helps regulate heart rhythm and supports the proper function of muscles, including the heart. It helps transmit electrical impulses that control your heart’s contraction and relaxation, which results in a steady heartbeat.
Additionally, potassium helps support normal blood pressure levels. It counteracts the effects of sodium (which can raise blood pressure when in excess), promoting vasodilation and reducing the risk of hypertension and related heart diseases.
Getting enough potassium in your diet, but not too much is key for overall heart health. The best way to ensure you’re getting what you need is to maintain a balanced diet including a variety of nutrient-dense foods.
On another note, many people think that if their blood levels of potassium are normal that means they’re eating enough potassium, but that’s not necessarily true. Kidney function and potassium redistribution can influence blood levels regardless of dietary intake.
If your potassium levels are higher or lower than normal (because your body isn’t excreting it properly or you’re experiencing too much output from diuretic use) this can indicate a need to adjust your diet. Normal potassium is generally between 3.5 to 5.0 milliequivalents per liter (mEq/L).
Your potassium levels can also be influenced by things like medications and lifestyle factors. In other words, your potassium levels from a blood test don’t always reflect potassium adequacy in your diet. To evaluate your potassium needs and ensure adequacy, seeking guidance from a registered dietitian who can develop a personalized plan based on your medical history and individual circumstances is recommended.
Potassium and Heart Failure
In heart failure, maintaining adequate potassium levels is essential for regulating heart rhythm and preventing complications such as arrhythmias or even death. Potassium helps stabilize your heart’s electrical impulses.
Potassium supplementation may be recommended for some individuals with heart failure who are at risk of developing hypokalemia (low potassium levels) due to diuretic medications commonly used to manage fluid retention. However, supplementation should only be used when regulating your potassium levels to avoid high or low values, and only under professional guidance.
However, it’s critical to monitor potassium levels carefully. Both low and high potassium can exacerbate heart failure symptoms and increase the risk of complications.
Potassium-Rich Foods List and Dietary Recommendations
Potassium is a nutrient you must get through your diet because over-the-counter supplements are capped at 99 mg doses. This is significantly lower than our daily needs, which are 4700 mg.
Recent data from the National Health and Nutrition Examination Survey (NHANES) shows that most Americans eat significantly more sodium than needed and often fall short of their daily potassium needs. Most of our sodium comes from ultra-processed foods like packaged and frozen foods, some canned foods, convenience/fast foods, and added salt during cooking.
So while you’re paying attention to (and possibly reducing) sodium intake, it’s important to regularly include sources of potassium.
The best way to meet your daily needs is to eat a diet including a variety of foods that have potassium, like:
- Bananas
- Oranges
- Avocados
- Spinach
- Potatoes
- Tomatoes
- Beans
- Lentils
In addition to knowing what food has potassium, note that certain cooking methods can affect how much you’ll get from foods. Choosing methods that involve minimal water and shorter cooking times, like steaming or microwaving, as well as grilling and roasting, can help retain more of the potassium in foods compared to frying and boiling in water.
Lifestyle Factors Affecting Potassium and Heart Health
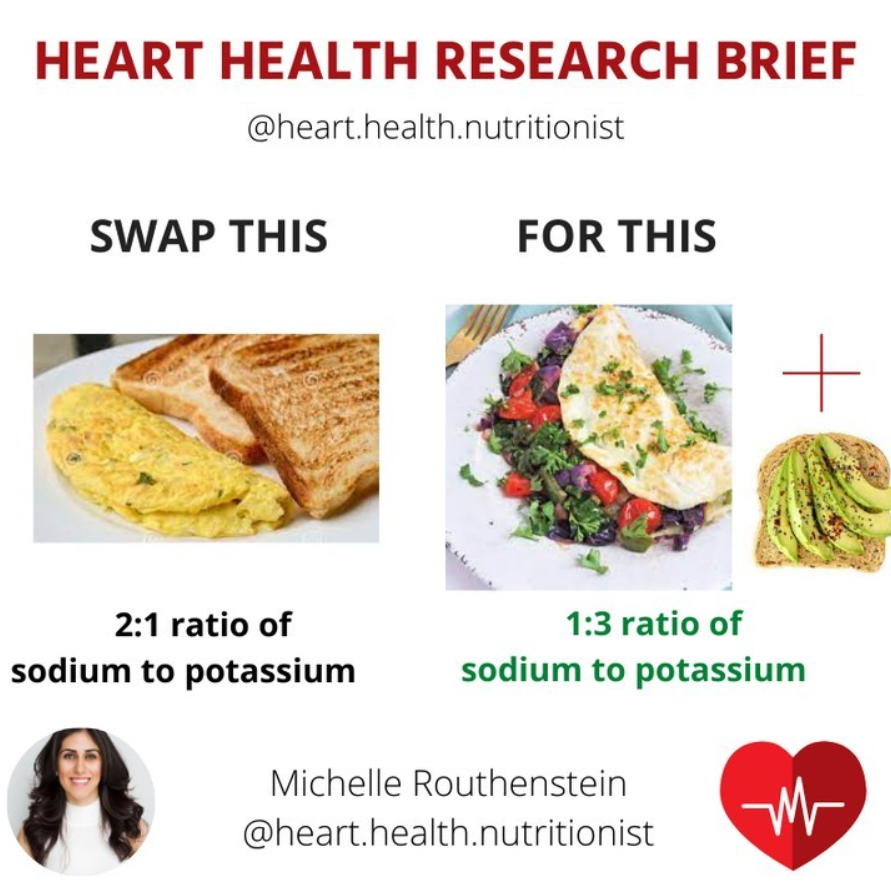
Sodium-Potassium Ratio
To help improve blood pressure, one of the many things you can do is focus on the sodium-to-potassium ratio. Sodium and potassium work in tandem in the body to control blood pressure.
Both are important components of heart health and the ratio is what may matter most. The guidelines indicate an optimal sodium-to-potassium ratio is 1:3 or 1:2, meaning 2-3x more potassium than sodium.
To maintain a healthy ratio, eat a diet rich in potassium-containing foods while reducing sodium intake from ultra-processed and high-sodium foods.
Many of my clients have questioned whether those following a salt-restricted diet should use a salt substitute, which I actually wouldn’t recommend. Salt substitutes are mainly potassium chloride.
Potassium chloride can be dangerous for people with cardiovascular, kidney, or liver issues because when used in high dosages, it can lead to high levels of potassium in the blood which can cause harmful side effects.
Exercise
Intense or prolonged exercise can increase potassium loss through sweat. Have you ever gotten really sweaty and tasted salt on your skin? There’s probably some potassium in there, too.
At the same time, regular moderate exercise also enhances potassium uptake into your muscle cells. This promotes healthy potassium redistribution and overall balance.
Hydration and consuming rich potassium foods, especially shortly after tough workouts, can help restore optimal potassium levels and support muscle function.
Alcohol
Alcohol can indirectly affect potassium by impairing dietary choices. Excessive alcohol intake can displace potassium-rich foods in your diet as well as lead to dehydration, which may disrupt electrolyte balance.
Chronic alcohol abuse can also impair kidney function, potentially affecting potassium excretion and increasing the risk of electrolyte imbalances.
Potassium-Sparing Medications
Potassium-sparing medications are a class of drugs commonly used to manage hypertension and heart failure. They help keep your potassium levels normal by preventing it from being lost in your urine.
If you normally consume a high amount of potassium through your diet, it may need to be adjusted (but never eliminated) when on these medications. Always work with a registered dietitian to help you determine your dietary needs.
Client Success Story
A 35-year-old woman came to see me for guidance on adding nutrition to her medical therapy.
She had systolic heart failure with dilated cardiomyopathy, diagnosed after she gave birth to her son. We worked closely together in my VIP program.
She was winded and tired after simple activities but had a normal BMI and waist circumference. Her blood work showed she had iron deficiency anemia, common in heart failure. She also had Sjogren’s, an inflammatory condition that adds to a typical inflammatory state of heart failure.
She was taking Spironolactone, a potassium-sparing medicine, so we carefully addressed her potassium and nutrient deficiencies and implemented an easy heart-healthy diet.
In 4 months, her energy improved, allowing moderate exercise without shortness of breath. She experienced improvements in bowel health, inflammation, iron deficiency, and overall nutrient sufficiency.
The Bottom Line: Potassium and the Heart
Your heart needs adequate potassium (not too much, not too little) to function properly, including for normal blood pressure and heart rhythm. The best way to meet your daily needs for potassium, which is typically around 4700 mg (unless you have kidney issues or are on potassium-sparing medications), is to eat a diet rich in potassium foods like certain fruits, vegetables, and whole grains, versus supplements. Consult your dietitian to determine your appropriate potassium goals from food.
Interested in individualized guidance around science-based nutrition for heart health, including potassium? Consider 1:1 counseling or joining my Heart Health Optimization group coaching program.
References
- Weaver CM. Potassium and health. Adv Nutr. 2013;4(3):368S-77S. Published 2013 May 1. doi:10.3945/an.112.003533
- Filippini T, Naska A, Kasdagli MI, et al. Potassium Intake and Blood Pressure: A Dose-Response Meta-Analysis of Randomized Controlled Trials. J Am Heart Assoc. 2020;9(12):e015719. doi:10.1161/JAHA.119.015719
- Chiamvimonvat N, Chen-Izu Y, Clancy CE, et al. Potassium currents in the heart: functional roles in repolarization, arrhythmia and therapeutics. J Physiol. 2017;595(7):2229-2252. doi:10.1113/JP272883
- Zhang JL, Yu H, Hou YW, et al. Impact of long-term potassium supplementation on thiazide diuretic-induced abnormalities of glucose and uric acid metabolisms. J Hum Hypertens. 2018;32(4):301-310. doi:10.1038/s41371-018-0036-3
- Vaudin A, Wambogo E, Moshfegh AJ, Sahyoun NR. Sodium and Potassium Intake, the Sodium to Potassium Ratio, and Associated Characteristics in Older Adults, NHANES 2011-2016. J Acad Nutr Diet. 2022;122(1):64-77. doi:10.1016/j.jand.2021.06.012
- Coe S, Spiro A. Cooking at home to retain nutritional quality and minimise nutrient losses: A focus on vegetables, potatoes and pulses. Nutr Bull. 2022;47(4):538-562. doi:10.1111/nbu.12584
- Levings JL, Gunn JP. The imbalance of sodium and potassium intake: implications for dietetic practice. J Acad Nutr Diet. 2014;114(6):838-841. doi:10.1016/j.jand.2014.02.015
- Mohn ES, Kern HJ, Saltzman E, Mitmesser SH, McKay DL. Evidence of Drug-Nutrient Interactions with Chronic Use of Commonly Prescribed Medications: An Update. Pharmaceutics. 2018;10(1):36. Published 2018 Mar 20. doi:10.3390/pharmaceutics10010036
- Baj J, Flieger W, Teresiński G, et al. Magnesium, Calcium, Potassium, Sodium, Phosphorus, Selenium, Zinc, and Chromium Levels in Alcohol Use Disorder: A Review. J Clin Med. 2020;9(6):1901. Published 2020 Jun 18. doi:10.3390/jcm9061901
