During pregnancy, most women are focused on having a healthy baby. But mom’s health matters as well. There are certain medical concerns that might pop up during or after your pregnancy that can put the mom’s health at risk. One of these conditions is postpartum cardiomyopathy, a heart condition that impacts your heart muscle and increases your risk of heart disease.
What is cardiomyopathy?
Cardiomyopathy refers to conditions that affect your heart muscle, also known as your myocardium. This makes it harder for your heart to pump blood, impacting your heart function.
Your heart is made up of 4 chambers including the left atrium, right atrium, left ventricle, and right ventricle. The left and right atrium receive blood from your veins while the ventricles pump blood out of your body.
With postpartum cardiomyopathy, the chambers of the heart can enlarge. Additionally, there can be a decrease in the percentage of blood ejected from the heart with each contraction. This can cause a backup of fluid in the lungs leading to symptoms like shortness of breath, leg swelling, and chest pain.
Depending on the type of cardiomyopathy that you have, your heart muscle may become thick, ridged, or enlarged. This can lead to symptoms that may include irregular heartbeat, heart palpitations, shortness of breath, and postpartum heart failure.
Peripartum cardiomyopathy can occur during the last month of pregnancy while postpartum cardiomyopathy may develop shortly after your pregnancy. They can both lead to a weakening of the pumping chambers of the heart which can cause the muscles to become thinner, leading to abnormal heart contractions.
This condition is relatively rare; according to the American Heart Association, roughly 1,000 to 1,300 women develop the condition in the U.S. each year.1
Symptoms of postpartum cardiomyopathy
Symptoms like shortness of breath and leg swelling are quite common during pregnancy. Therefore, it’s important to be aware of the specific signs, symptoms, and risk factors that may be an indication that something more serious is going on.
In severe cases of postpartum cardiomyopathy, the heart may not be able to provide enough oxygen for the body’s organs. The lack of oxygen puts the lungs, liver, and kidneys at risk. In these rare cases, a woman may need a device to support her heart muscle and to help prevent a postpartum heart attack.
Peripartum and postpartum cardiomyopathy symptoms often overlap with those of a normal pregnancy.
Common symptoms may include:
- Extreme fatigue
- Irregular heartbeat
- Heart palpitations
- Increased urination at night
- Shortness of breath with activity
- Shortness of breath when lying flat
- Swollen lower legs and ankles
- Swollen neck veins
- Low blood pressure
- Chest pain
If you are at risk or experience any of these symptoms it’s important to speak with your healthcare provider.
Postpartum cardiomyopathy risk factors
During pregnancy, your heart pumps up to 50% more blood to help transfer oxygen and nutrients to your baby. While the underlying cause of postpartum cardiomyopathy is unclear, it may be a result of the heart pumping extra blood combined with other risk factors. 2
Additionally, studies show that women who have had postpartum cardiomyopathy also have inflammation of the heart muscle. This risk factor may be related to a viral illness or an abnormal immune response. 3
The following are risk factors for postpartum cardiomyopathy:
- Older maternal age (30+)
- History of myocarditis
- History of heart attack
- History of heart valve dysfunction
- High blood pressure
- Multiple pregnancies
- Multifetal pregnancy (twins, triplets)
- Use of certain medications to prevent premature labor
- African American descent
- Poor nutrition
- Excess alcohol intake
- Smoking
- Obesity
- Diabetes
A 2019 study suggests that there is a genetic component to postpartum cardiomyopathy as cases of the condition often cluster in families. 4
How to manage postpartum cardiomyopathy
Managing postpartum cardiomyopathy includes a science based heart healthy diet to help reduce complications and medication therapy (managed by your healthcare provider).
Women with the condition may have to reduce their salt diet to help improve blood pressure and reduce fluid retention. However, nutrition therapy for a heart healthy diet goes far beyond reducing your intake of salt or eliminating certain foods.
Adding therapeutic foods to your diet can help enhance heart functioning, improve blood pressure control, and address underlying issues like inflammation and oxidative stress that cause the heart to overwork and cause a negative progression.
Some examples include:
- Isoflavones are plant compounds found in foods like tofu and flaxseed, that have been shown to help reduce arterial stiffness and assist with better blood flow. 4
- Sulfur containing foods that enhance the master antioxidant pathway, the glutathione pathway. Some of these foods include broccoli, avocado and garlic.
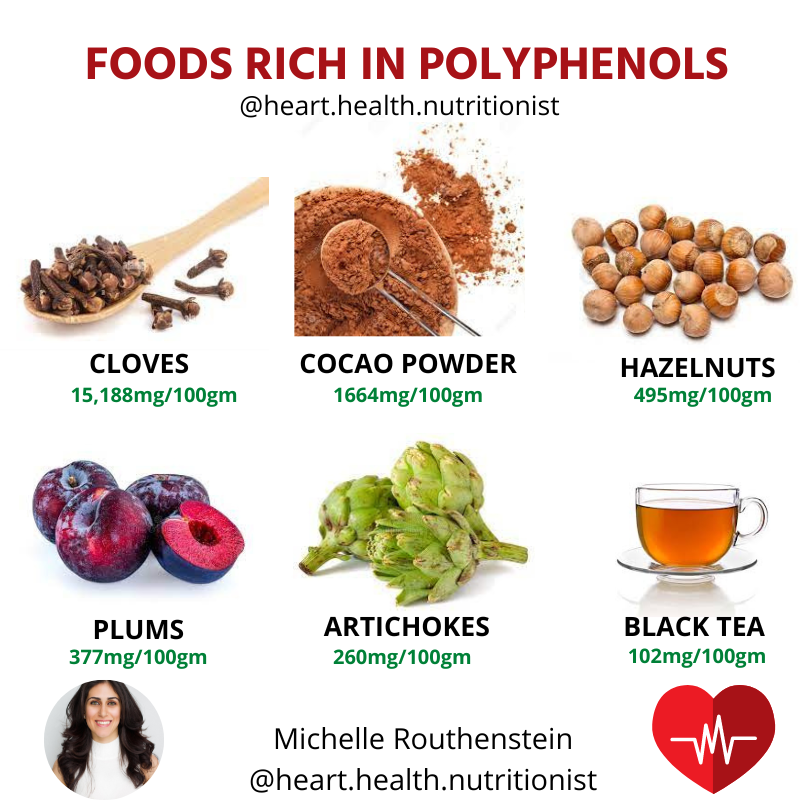
- Polyphenols are found in certain foods that may help address inflammation.5 These include:
- Berries (strawberries, raspberries, blueberries)
- Beans (white beans and black beans)
- Hazelnuts
- Black tea
- Cloves
- Cocao powder
- Whole grains
- Asparagus
The balance of all of your nutrients is also essential for management of cardiomyopathy and individual needs for protein, carbohydrates, fat, and micronutrients need to be assessed. If you are looking for personalized support on your heart health journey, consider asking for help by a qualified registered dietitian who specializes in cardiovascular disease.
Medication Management of Postpartum Cardiomyopathy
Postpartum cardiomyopathy is treated in a similar way as other forms of cardiomyopathy. However, managing the condition may be different depending on if the condition occurs before or after the baby is born. Either way, the goal of treatment is to reduce extra fluid from collecting in the lungs to help keep pressure off of the heart.
There are some medications that are used to help manage the condition. For example, your doctor may prescribe an ACE (angiotensin converting enzyme) inhibitor. This type of medication can help dilate your blood vessels allowing your heart to work more efficiently.
It is important to note that ACE inhibitors cannot be used during pregnancy. This type of drug can negatively affect your baby’s kidneys, therefore your doctor will need to look for an alternative if it starts during pregnancy. 5
Another medication your doctor might prescribe if you have postpartum cardiomyopathy is a beta-blocker. Beta-blockers, which can be used during pregnancy, help to decrease your heart rate and blood pressure.
Diuretics, or “water pills” may also be used to treat the condition during or after pregnancy. This medication helps manage symptoms of postpartum cardiomyopathy by helping to reduce fluid retention.
It is important to note that some of these medications can deplete or hold onto essential micronutrients which can impact optimal heart health, so a personalized assessment of your nutrients to ensure you are achieving all of the appropriate amounts of nutrients your heart needs for properly functioning is recommended.
Supporting your heart health postpartum
If you are at high risk for postpartum cardiomyopathy, or if you are concerned about your heart health prior, during or after pregnancy, a supportive science based heart optimization program can help. In my 6-week heart optimization group program, I guide you on how to implement science based heart health strategies to improve your heart health, while being a part of a supportive community of individuals who may be going through a similar journey as you are.
If you are pregnant or postpartum and have been diagnosed with cardiomyopathy, you may benefit from meeting with 1 on 1 with registered dietitian who specializes in heart disease. With my extensive experience in cardiovascular care and as a mother myself, I can develop a science-based individualized plan to help you achieve your goals to stay healthy during pregnancy and beyond.
Finding the right support and evidence-based information can help protect your heart, protect your baby, and reduce your risk of heart complications down the road.
References:
- American Heart Association: Peripartum Cardiomyopathy, Assessed June 9, 2022. https://www.heart.org/en/health-topics/cardiomyopathy/what-is-cardiomyopathy-in-adults/peripartum-cardiomyopathy-ppcm#:~:text=Peripartum%20cardiomyopathy%20(PPCM)%2C%20also,literally%20means%20heart%20muscle%20disease
- Davis M, Duvernoy C. Peripartum Cardiomyopathy: Current Knowledge and Future Directions. Women’s Health. July 2015:565-573. doi:10.2217/WHE.15.15
- Mubarik A, Chippa V, Iqbal AM. Postpartum Cardiomyopathy. [Updated 2022 Apr 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534770/
- Ma, L., Liu, G., Ding, M., Zong, G., Hu, F. B., Willett, W. C., Rimm, E. B., Manson, J. E., & Sun, Q. (2020). Isoflavone Intake and the Risk of Coronary Heart Disease in US Men and Women: Results From 3 Prospective Cohort Studies. Circulation, 141(14), 1127–1137. https://doi.org/10.1161/CIRCULATIONAHA.119.041306
- Jiang S, Liu H, Li C. Dietary Regulation of Oxidative Stress in Chronic Metabolic Diseases. Foods. 2021;10(8):1854. Published 2021 Aug 11. doi:10.3390/foods10081854
- Honigberg M C, Givertz M M. Peripartum cardiomyopathy BMJ 2019; 364 :k5287 doi:10.1136/bmj.k5287
- Buawangpong, N, Teekachunhatean, S, Koonrungsesomboon, N. Adverse pregnancy outcomes associated with first-trimester exposure to angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers: A systematic review and meta-analysis. Pharmacol Res Perspect. 2020;e00644. https://doi.org/10.1002/prp2.644