A widowmaker heart attack is the most dangerous type of heart attack. However, understanding why widowmaker heart attacks happen and what you can do to prevent one can make it feel a bit less scary.
In this article, we cover what a widowmaker heart attack is as well as the risk factors and symptoms. But most importantly we will also discuss what you can do to take control of your health and potentially prevent this dangerous heart attack.
What is a widowmaker heart attack?
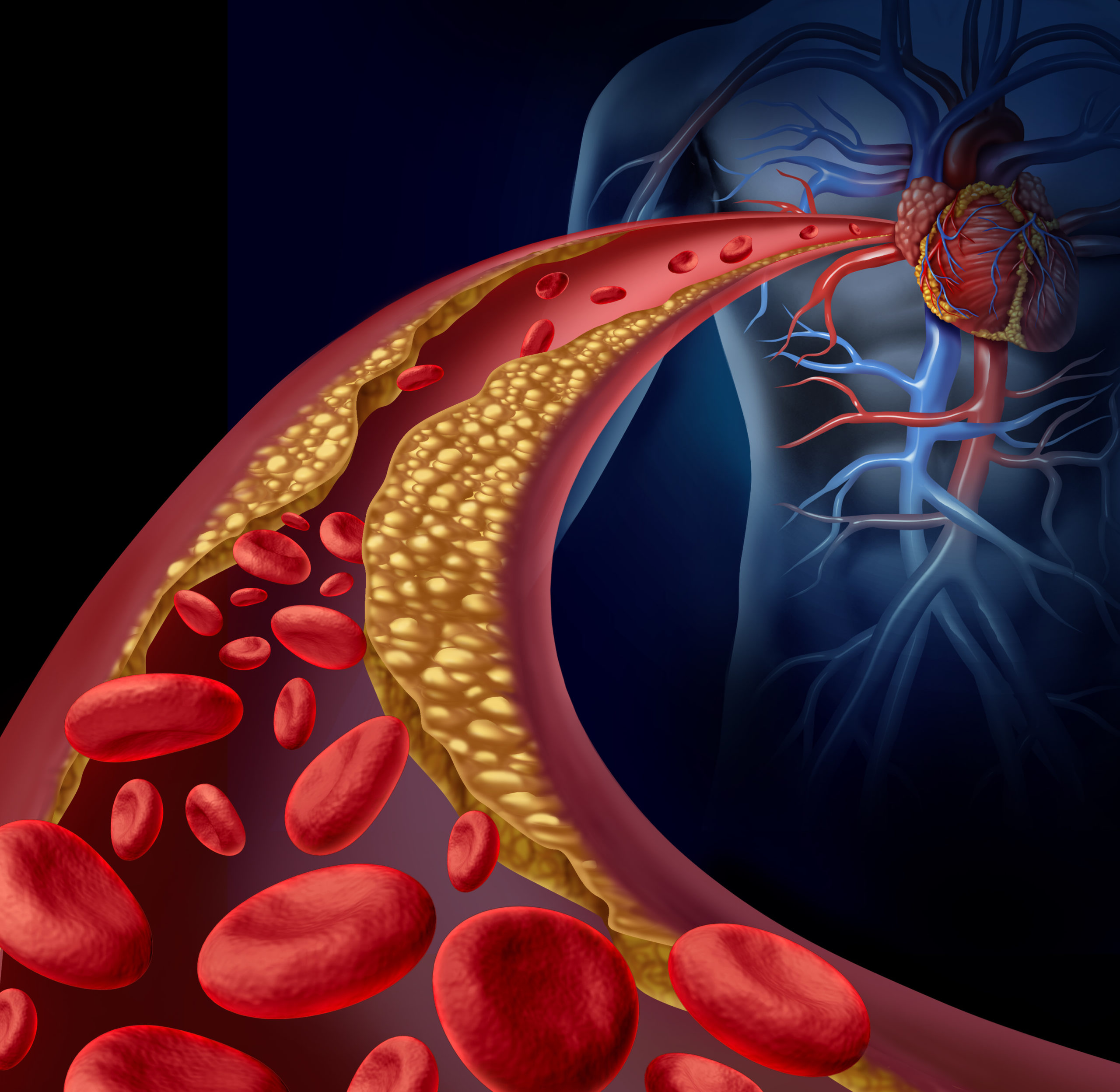
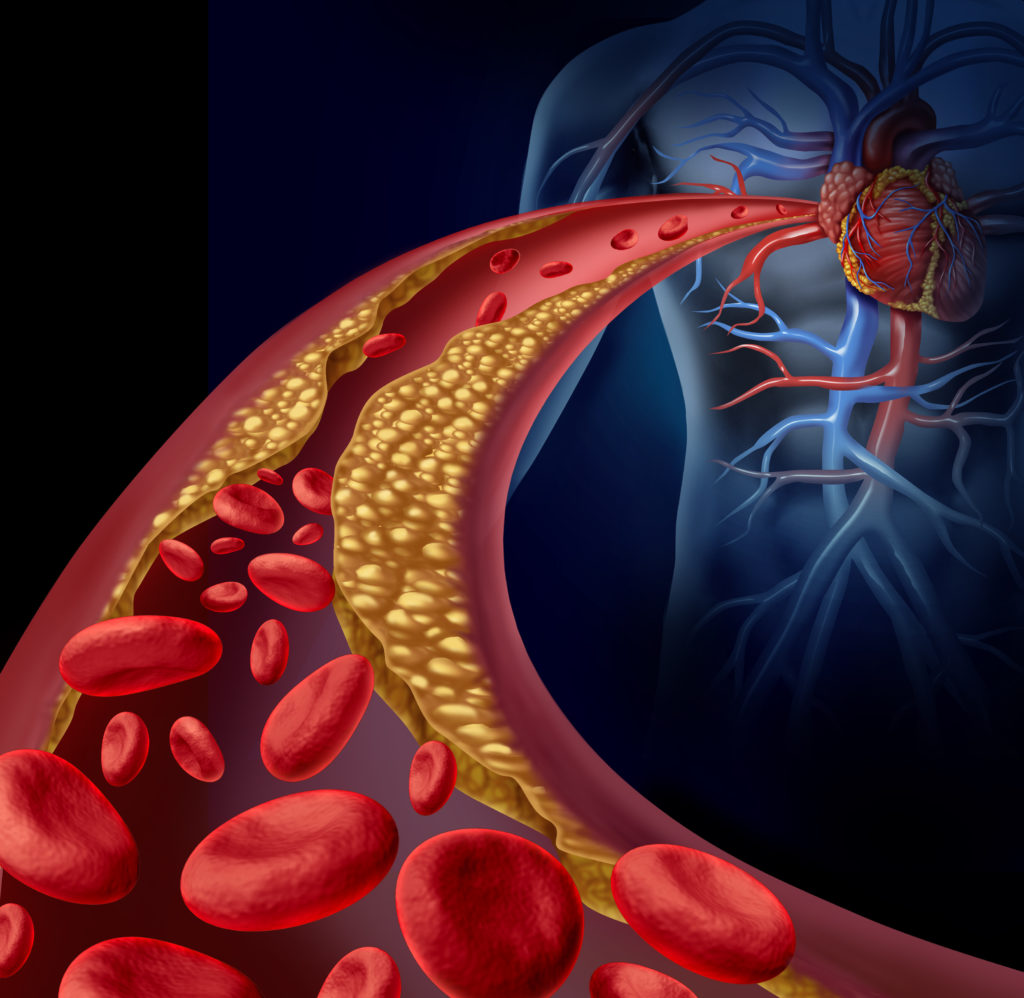
A widowmaker is more formally known as an anterior ST-segment elevation myocardial infarction (STEMI). It is the most dangerous type of heart attack, occurring when the left anterior descending (LAD) artery is completely blocked after a plaque rupture.
The LAD artery supplies oxygenated blood to the interventricular septum between the left and right ventricles of the heart as well as the anterior left ventricle. The LAD artery can become subject to arterial plaque buildup which can cause narrowing and stiffness in the artery.1
Arterial plaque is the result of cholesterol, cellular waste, fatty substances, and fibers building up along the inner arterial wall. Eventually, due to inflammation, oxidation, stress and weakening of the plaque structure, an arterial plaque can rupture and cause a blockage to the arteries, also known as coronary thrombosis.2
Because the LAD artery is responsible for bringing oxygenated blood to half of the heart, a blockage can result in inadequate blood flow, myocardial injury, and even disruptions in the heart’s normal contraction.
Risk factors and symptoms
Despite its moniker of the “widowmaker,” a STEMI can affect people of any gender. Men are more likely to have a widowmaker heart attack than women, but the outcomes can differ greatly.
Widowmaker heart attack survival rate depends on how quickly one can get medical attention. The 30-day mortality rate for a widowmaker heart attack is between 2.5 to 10%, with the mortality rate being slightly higher for women than men.3, 4
Risk factors of a widowmaker heart attack
The American Heart Association recognizes several risk factors that can increase a person’s risk for a widowmaker heart attack 5:
- Diabetes
- Hypertension
- Smoking
- Stress
- Weight
- Family history of coronary heart disease
- Dyslipidemia (an imbalance of cholesterol and/or triglycerides)
- Age – men aged 45 years and older and women aged 55 years and older are at higher risk
Symptoms of a widowmaker heart attack
Symptoms of a STEMI or widowmaker heart attack are similar to other heart attacks. A widowmaker heart attack can include one or more of the following symptoms 6:
- Pain or discomfort in the neck, jaw, back, arms, or stomach
- Shortness of breath
- Chest pain, tightness, or discomfort
- Lightheadedness, weakness, or feeling faint
- Breaking out in a cold sweat
- Nausea
Widowmaker prevention
A widowmaker heart attack can sound intimidating, but there are things you can do to prevent them no matter what your risk is. With some lifestyle changes and regular screenings, you can take control of your health and prevent a widowmaker heart attack.
Preventative screenings
Individuals who are at risk for heart disease between the ages of 40-70 years and those with a family history of high cholesterol can benefit from calcium-score screening. A Coronary Calcium (CAC) scan is a helpful tool for monitoring the health of your arteries and risk for a widowmaker heart attack.
A CAC scan uses a CT scan to provide pictures of your heart’s arteries and calculates calcium deposits present in the heart. A higher calcium score may indicate a plaque buildup and an increased risk for a heart attack. If significant plaque buildup is found in the LAD, then this may indicate the potential for a widowmaker heart attack.
A heart-healthy diet
A great number of different food patterns like a plant-based diet or Mediterranean diet can be protective against a widowmaker heart attack. At the root of all things, a heart-healthy diet is one that is well-balanced in macronutrients, micronutrients, and therapeutic foods to help your heart work optimally.
Research shows that high-quality diets consisting of a variety of foods significantly reduce the risk of heart disease. Beyond providing vitamins, minerals, and macronutrients, various foods have compounds that give additional health benefits. 7
For instance, plant polyphenols are phytochemicals that can support healthy blood vessels, normal cholesterol levels, and protect against inflammation. Some examples of polyphenols that have been well-studied for their impact on heart health include resveratrol in blueberries, epigallocatechin gallate (EGCG) from tea, curcumin found in turmeric, and quercetin.8
Plant sterols and stanols are plant substances that are structurally similar to cholesterol. They are effective for managing cholesterol levels due to their ability to inhibit the absorption of cholesterol by the body.9
Phytoestrogens like lignans and isoflavones from flaxseed and soy, respectively, can also protect women from cardiovascular disease. 10
To get the most out of your diet, focus on adding in nutrient-rich therapeutic foods your body needs to achieve improved blood pressure control, reduced inflammation and oxidative stress, and overall improved heart function. I discuss all of these foods that would benefit cardiovascular health in my 6 week heart optimization group program.
Exercise
Regular exercise can support the flexibility of your arteries and reduce the risk of atherosclerosis. Current guidelines recommend that healthy adults get 150 minutes of moderate-intensity exercise weekly.
Two types of exercise that are shown to be effective for heart health include aerobic (cardio) and resistance (strength) exercises. Aerobic exercises include exercises that use large muscle groups and are maintained for a while, including running, hiking, swimming, dancing, and biking. Resistance exercises are typically done for shorter durations of time and include some weight resistance such as weight lifting, squats and lunges, push-ups, and similar exercises. 11
Studies find that doing both resistance and aerobic exercise in your routine may be the most effective for losing weight, improving cardiorespiratory fitness, and increasing fat loss compared to resistance or aerobic exercise alone. 12
Medication
Taking medications as needed and as prescribed for normal blood clotting, blood pressure, and blood lipid levels can reduce the risk of further heart disease and complications. If choosing to add supplements to your diet, you should always consult with your health care team to ensure it is personalized for you and takes into account your medical history, diet, and medications you use.
Monitoring labs
Along with CAC scans, keeping up to date with your medical labs can help you know when to seek additional support. Important labs to monitor during your regular doctor’s visits include blood pressure, hsCRP, LDL (advanced if available), triglycerides, and hemoglobinA1c, to name a few.. I created a self-paced course to help you learn more about the other lab tests that may help you better assess your heart health.
Weight management
Managing your weight can reduce your risk for heart attack and other chronic conditions that can cause damage to your vascular system. People with a BMI of 25 or higher generally have a greater risk of getting a widowmaker heart attack. Losing 5-10% of your body weight can significantly reduce certain cardiovascular risks like triglyceride levels, LDL and total cholesterol. 13
In addition to managing your overall weight, where your weight settles has an impact on your cardiovascular risk. Waist circumference is an anthropometric measurement that correlates with visceral adiposity, or fat that surrounds the internal organs. A higher waist circumference is associated with a great risk of metabolic disease because this type of fat is more metabolically active and is usually associated with inflammation and insulin resistance.
The current guidelines for waist circumference notes that a waist circumference >102 cm (40 in) in men or >88 cm (35 in) in women is associated with greater health risks. However, these guidelines are not universal and waist circumference thresholds may differ based on BMI category and ethnicity. 14
Smoking cessation
Smoking is a major risk for the development of arterial plaques and heart attacks. Smoking decreases blood flow to the heart and increases inflammation, which can promote plaque formation.
Diabetes management
Diabetes is a risk factor for heart attacks due to its impact on the health of your vascular system. Excess blood glucose can decrease the elasticity of your blood vessels, reduce blood flow, and increase high blood pressure risk. Managing your blood sugar through diet and medications as needed can minimize the damage to the blood vessels and arteries of your heart.
Take control of your health
The journey to a healthy heart can be overwhelming and confusing to take on by yourself. As a registered dietitian with years of specialized experience in cardiac care, I have helped many overcome the roadblocks that make managing your health difficult.
My 6-week heart optimization group program can help you understand the underlying root causes of heart disease and how to reduce your risk of a future cardiac event. I also offer 1 on 1 services to help reduce your risk of heart diseases like widowmaker heart attacks through science-based, personalized nutrition.
References
- Rehman I, Kerndt CC, Rehman A. Anatomy, Thorax, Heart Left Anterior Descending (LAD) Artery. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482375/
- Palasubramaniam J, Wang X, Peter K. Myocardial Infarction-From Atherosclerosis to Thrombosis. Arterioscler Thromb Vasc Biol. 2019;39(8):e176-e185. doi:10.1161/ATVBAHA.119.312578
- Akbar H, Foth C, Kahloon RA, et al. Acute ST Elevation Myocardial Infarction. [Updated 2021 Aug 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532281/
- Cenko E, Yoon J, Kedev S, et al. Sex Differences in Outcomes After STEMI: Effect Modification by Treatment Strategy and Age. JAMA Intern Med. 2018;178(5):632-639. doi:10.1001/jamainternmed.2018.0514
- “Understanding Your Risks to Prevent a Heart Attack.” American Heart Association. Last Updated 30 June 2016. Available from: https://www.heart.org/en/health-topics/heart-attack/understand-your-risks-to-prevent-a-heart-attack
- “Warning Signs of a Heart Attack.” American Heart Association. Available from: https://www.heart.org/en/health-topics/heart-attack/warning-signs-of-a-heart-attack
- Petersen KS, Kris-Etherton PM. Diet Quality Assessment and the Relationship between Diet Quality and Cardiovascular Disease Risk. Nutrients. 2021;13(12):4305. Published 2021 Nov 28. doi:10.3390/nu13124305
- Khurana S, Venkataraman K, Hollingsworth A, Piche M, Tai TC. Polyphenols: benefits to the cardiovascular system in health and in aging. Nutrients. 2013;5(10):3779-3827. Published 2013 Sep 26. doi:10.3390/nu5103779
- Trautwein EA, Vermeer MA, Hiemstra H, Ras RT. LDL-Cholesterol Lowering of Plant Sterols and Stanols-Which Factors Influence Their Efficacy?. Nutrients. 2018;10(9):1262. Published 2018 Sep 7. doi:10.3390/nu10091262
- Rietjens IMCM, Louisse J, Beekmann K. The potential health effects of dietary phytoestrogens. Br J Pharmacol. 2017;174(11):1263-1280. doi:10.1111/bph.13622
- Patel H, Alkhawam H, Madanieh R, Shah N, Kosmas CE, Vittorio TJ. Aerobic vs anaerobic exercise training effects on the cardiovascular system. World J Cardiol. 2017;9(2):134-138. doi:10.4330/wjc.v9.i2.134
- Schroeder EC, Franke WD, Sharp RL, Lee DC. Comparative effectiveness of aerobic, resistance, and combined training on cardiovascular disease risk factors: A randomized controlled trial. PLoS One. 2019;14(1):e0210292. Published 2019 Jan 7. doi:10.1371/journal.pone.0210292
- Brown JD, Buscemi J, Milsom V, Malcolm R, O’Neil PM. Effects on cardiovascular risk factors of weight losses limited to 5-10. Transl Behav Med. 2016;6(3):339-346. doi:10.1007/s13142-015-0353-9
- Ross R, Neeland IJ, Yamashita S, et al. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16(3):177-189. doi:10.1038/s41574-019-0310-7