When you’re concerned about your heart health, it’s important to understand the difference between events like a heart attack and conditions like heart failure. While these two seem similar, they’re not the same. Recognizing their distinct characteristics and implications can be vital for getting the right medical intervention.
What is a Heart Attack?
A heart attack, also known as myocardial infarction, occurs when the blood flow to a part of the heart is blocked, often by a blood clot, causing damage to the heart muscle.
When there’s a blockage preventing normal blood flow to your heart, it will start beating irregularly. If normal blood flow isn’t restored quickly enough, that part of your heart muscle can die and form scar tissue. Ultimately, this means your heart cannot pump blood throughout your body as well as it did before.
Knowing the symptoms of a heart attack can help you react quickly if you think you, or someone you love, is having one.
Heart Attack Causes
The leading cause of a heart attack is the development of atherosclerosis, or plaque buildup, in the arteries that surround the heart. Atherosclerosis can happen in any of your arteries or blood vessels throughout the body. However, when it happens in the arteries of the heart then it can lead to a heart attack.
The good news is that many of your risk factors for having a heart attack are modifiable, which means you have the power to help protect yourself. In fact, an estimated 80% of cardiovascular diseases, including heart attacks and strokes, are preventable through lifestyle modification to optimize cholesterol, blood pressure, and weight.
Other causes of a heart attack include:
- A spasm in an artery of the heart
- Spontaneous Coronary Artery Dissection – when there is a tear in one of the arteries of the heart
A heart attack can be a stand-alone event, or it may lead to heart failure.
Heart Attack Symptoms
Many of us associate having a heart attack with the typical symptoms we see in movies, where the person clutches their chest and falls to the ground. However, it’s not always this obvious.
Some of the most common symptoms of a heart attack include:
- Discomfort in the jaw, neck, or back
- Weakness or lightheadedness
- Chest pain or discomfort
- Chest pain that travels from the left arm to the neck
- Arm or shoulder discomfort
- Shortness of breath with or without chest pain
- Sweating
- Nausea
- Vomiting
- Abnormal heartbeat
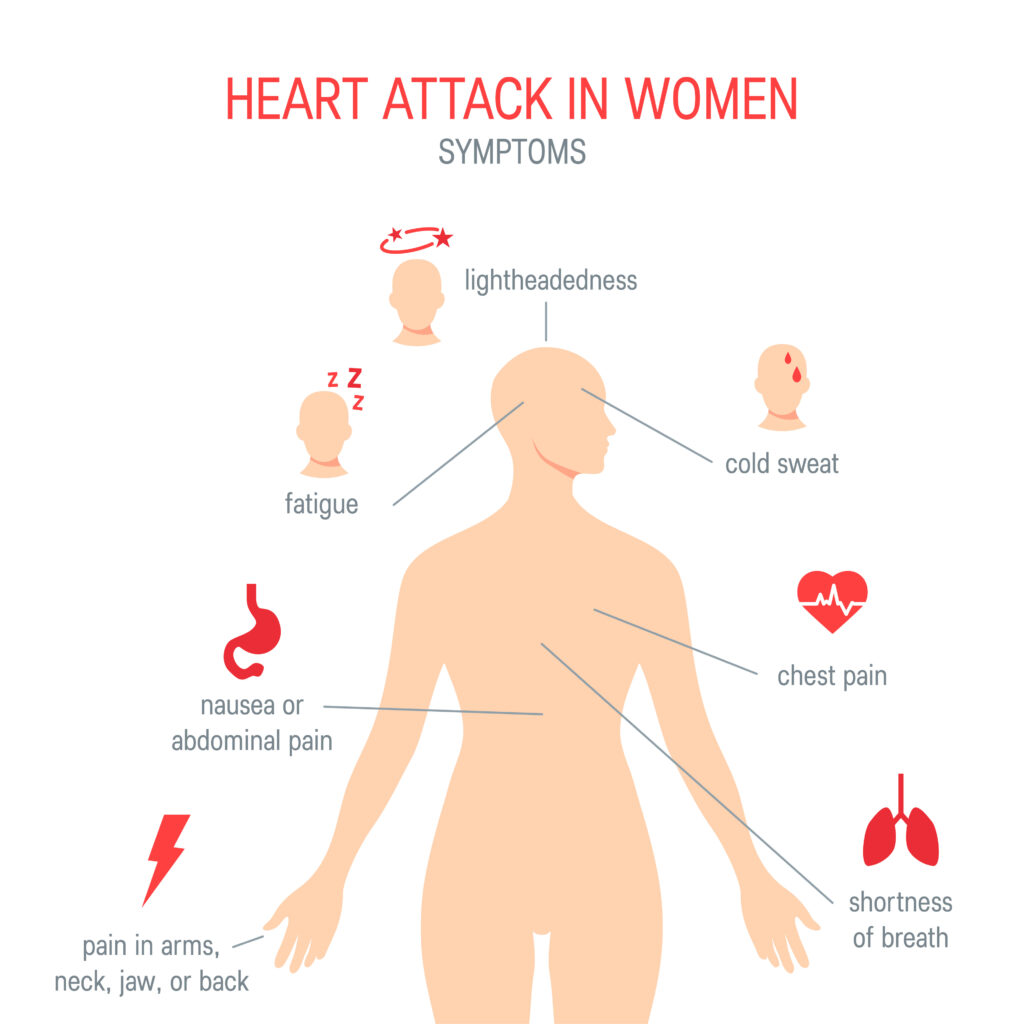
However, symptoms of heart attack in men can manifest very differently than those in women. This is one of the main reasons why there can be differences in how having a heart attack is recognized and treated. I’m on the medical advisory board committee of the National Menopause Foundation and one of the things I emphasize is understanding the differing symptoms and signs in women versus men.
Men typically experience the classic symptoms of a heart attack, such as intense chest pain or pressure, which may radiate to the arms, neck, or jaw. They might also break out in a cold sweat, feel dizzy, or have shortness of breath.
While we don’t always suspect it, heart attacks in women under 40 can also occur. Unfortunately, women are more likely to exhibit less obvious symptoms. You may notice subtle symptoms such as unusual fatigue, nausea, shortness of breath, flu-like symptoms, indigestion, general feelings of scaredness or weakness, or discomfort in the chest, back, jaw, or upper stomach just below the ribs.
These atypical signs can often be mistaken for less serious conditions. It’s important to know your body and take “off” feelings seriously, regardless of age or gender.
Most importantly, if you or someone you know experiences any of the symptoms, help should be sought immediately – call 911 or get the person to the emergency room as quickly as possible.
What is Heart Failure?
Heart failure isn’t what it sounds like – that the heart has stopped working. What heart failure really means is that the heart isn’t working as well as it could. This is a chronic condition where the heart cannot pump blood effectively to meet the body’s needs.
There are two classifications of heart failure, each describing a different dysfunction of the heart:
- Preserved ejection fraction: The heart’s left ventricle pumps out a normal percentage of blood with each beat but the heart muscle is stiff and doesn’t fill properly, leading to symptoms of heart failure.
- Reduced ejection fraction: This occurs when the left ventricle is weakened and cannot contract effectively, resulting in a lower percentage of blood being pumped out and causing a different type of heart failure.
Heart failure develops over time for a variety of reasons, which we’ll cover below. Because the heart muscle isn’t working as well as it used to, it makes adaptations to try to keep up with the workload.
For example, some of the adaptations your heart makes include:
- Enlarging: The heart, particularly the left ventricle, gets bigger in an attempt to produce a greater contraction and to pump more blood to the body.
- Increasing muscle mass: Your heart builds more muscle to attempt to contract more strongly. This can help for a while.
- Contracting more frequently: This results in a rapid heart rate because the heart is trying to keep up by contracting more times each minute than it used to.
Not surprisingly, the heart isn’t the only part of the body that tries to make changes when under this kind of stress. Blood arteries and vessels throughout the body will narrow to compensate for the heart’s lower-strength contractions. This can be a problem if some of the arteries and vessels are narrowed due to atherosclerosis. They become easier to block.
Another adaption the body makes is to reduce blood flow to areas of the body, including tissues, and organs that are less important than the heart.
If you aren’t sure if you’re experiencing heart failure or have concerns about your heart, you can talk with a cardiologist. They can test your heart’s ejection fraction by having an echocardiogram performed. These tests will give you the information you need about how efficiently your heart is working.
Heart Failure Causes
Heart failure has multiple causes and usually develops over a period of time. Below is a list of some things that can cause heart failure:
- Heart attack: a heart attack causes some of the heart muscle to die and leaves behind scar tissue. This decreases the ability of the heart to contract and pump blood.
- Coronary artery disease and cardiovascular disease: When the arteries that provide blood to the heart muscles are narrowed with plaque.
- Heart valve disease: If the heart valves aren’t working properly. This can be caused by rheumatic fever or other infections.
- Hypertension (AKA high blood pressure): The heart has to work harder to pump blood when blood pressure is high.
- Complications of diabetes: Over time, high blood sugar levels can damage blood vessels and nerves that control the heart, leading to an increased risk of plaque buildup and subsequent heart blockages.
- Certain chemotherapy drugs: Anthracyclines and HER2-targeted therapies are associated with an increased risk of heart failure due to their potential to cause damage to heart muscle cells. This cardiotoxicity can lead to reduced heart function and requires careful monitoring and management during and after cancer treatment.
While the causes are straightforward, the symptoms of heart failure can be vague.
Heart Failure Symptoms
You only start to feel symptoms of heart failure when the compensations and adaptations your body makes to help keep up stop working. The progression of heart failure can take years until it becomes noticeable. (Read more about the different stages of heart failure and when symptoms may appear here.)
Here is a list of the most common symptoms of heart failure. If you’re experiencing heart failure, you may:
- Feel short of breath when resting, during exercise, or even when lying flat.
- Have swelling in the abdomen, legs, and ankles due to a buildup of fluid.
- Be tired and weak.
- Experience a loss of appetite, nausea, and abdominal pain.
- Gain weight.
- Have a cough that produces blood-tinged sputum.
Preventing Heart Attacks and Heart Failure
Healthy lifestyle habits are some of the most impactful ways you can help prevent heart problems. If you’re diagnosed with a heart attack or heart failure, dietary approaches can be different as your care team will prioritize things necessary for the most immediate improvements.
It’s important to optimize your cardiometabolic health as well as address endothelial dysfunction for the prevention of heart attacks and heart failure. Endothelial dysfunction is triggered by a buildup of oxidative stress and can affect your ejection fraction, nitric oxide pathway, and blood pressure, making it much harder for your heart to work properly.
Addressing these requires a combination of optimizing the nutritional quality of your diet with stress management practices and regular physical activity. I work closely with my clients to help them address all of these issues that overtax their heart through science-based nutrition.
For example, we work on reducing ultra-processed, refined sugar and fatty foods and ensuring optimal nutrient intake through focusing on adding cardio-protective foods in their appropriate pairings, in addition to other individually tailored recommendations based on heart health labs and goals.
The Bottom Line: Heart Attack vs Heart Failure
A heart attack is when part of the heart loses blood flow, while heart failure is when the heart can’t pump as effectively as it used to. Both reduce the heart’s ability to pump blood through the body.
It’s critical to understand these differences between them, especially how their symptoms might appear in your life and the steps you can take to reduce your risk of developing them or worsening existing issues.
If you’re looking for more personalized guidance and actionable tips, consider joining my Heart Health Optimization group program. Here, we will talk about the prevention of both heart attacks and heart failure as we discuss the underlying root causes in lectures across 6 weeks (1 topic per week so you can have time to understand and implement them).
References
- World Heart Federation. CVD Prevention. Retrieved from https://world-heart-federation.org/what-we-do/prevention/#
- Saw J, Humphries K, Aymong E, et al. Spontaneous Coronary Artery Dissection: Clinical Outcomes and Risk of Recurrence. J Am Coll Cardiol. 2017;70(9):1148-1158. doi:10.1016/j.jacc.2017.06.053
- Lu L, Liu M, Sun R, Zheng Y, Zhang P. Myocardial Infarction: Symptoms and Treatments. Cell Biochem Biophys. 2015;72(3):865-867. doi:10.1007/s12013-015-0553-4
- Schulte KJ, Mayrovitz HN. Myocardial Infarction Signs and Symptoms: Females vs. Males. Cureus. 2023;15(4):e37522. Published 2023 Apr 13. doi:10.7759/cureus.37522
- Centers for Disease Control and Prevention. (2019). Awareness of Heart Attack Symptoms and Response Among Adults — United States, 2008, 2014, and 2017. Retrieved from https://www.cdc.gov/mmwr/volumes/68/wr/mm6805a2.htm?s_cid=mm6805a2_w
- Mehta LS, et al. (2016). Acute Myocardial Infarction in Women: A Scientific Statement From the American Heart Association. Circulation, 133(9). Retrieved from https://www.ahajournals.org/doi/10.1161/CIR.0000000000000351
- Redfield MM, Borlaug BA. Heart Failure With Preserved Ejection Fraction: A Review. JAMA. 2023;329(10):827-838. doi:10.1001/jama.2023.2020
- Murphy SP, Ibrahim NE, Januzzi JL Jr. Heart Failure With Reduced Ejection Fraction: A Review [published correction appears in JAMA. 2020 Nov 24;324(20):2107. doi: 10.1001/jama.2020.21736]. JAMA. 2020;324(5):488-504. doi:10.1001/jama.2020.10262
- Ziaeian, B., & Fonarow, G. C. (2016). Epidemiology and aetiology of heart failure. Nature Reviews Cardiology, 13(6), 368-378. https://doi.org/10.1038/nrcardio.2016.25
- Stenger M. (2023). Risk Factors for Incident Heart Failure Among Cancer Survivors Aged 18 to 39. The ASCO Post. https://ascopost.com/news/september-2023/risk-factors-for-incident-heart-failure-among-cancer-survivors-aged-18-to-39/#:
- New York Heart Association (NYHA) Classification. Specifications Manual for Joint Commission National Quality Measures (v2018A). Retrieved from https://manual.jointcommission.org/releases/TJC2018A/DataElem0439.html
- Zuchi C, Tritto I, Carluccio E, Mattei C, Cattadori G, Ambrosio G. Role of endothelial dysfunction in heart failure. Heart Fail Rev. 2020;25(1):21-30. doi:10.1007/s10741-019-09881-3
