Heart disease has been the top killer around the world for decades. Having heart disease refers to a number of conditions, such as coronary artery disease, which affects the flow of blood to your heart and can increase your risk of having a heart attack.
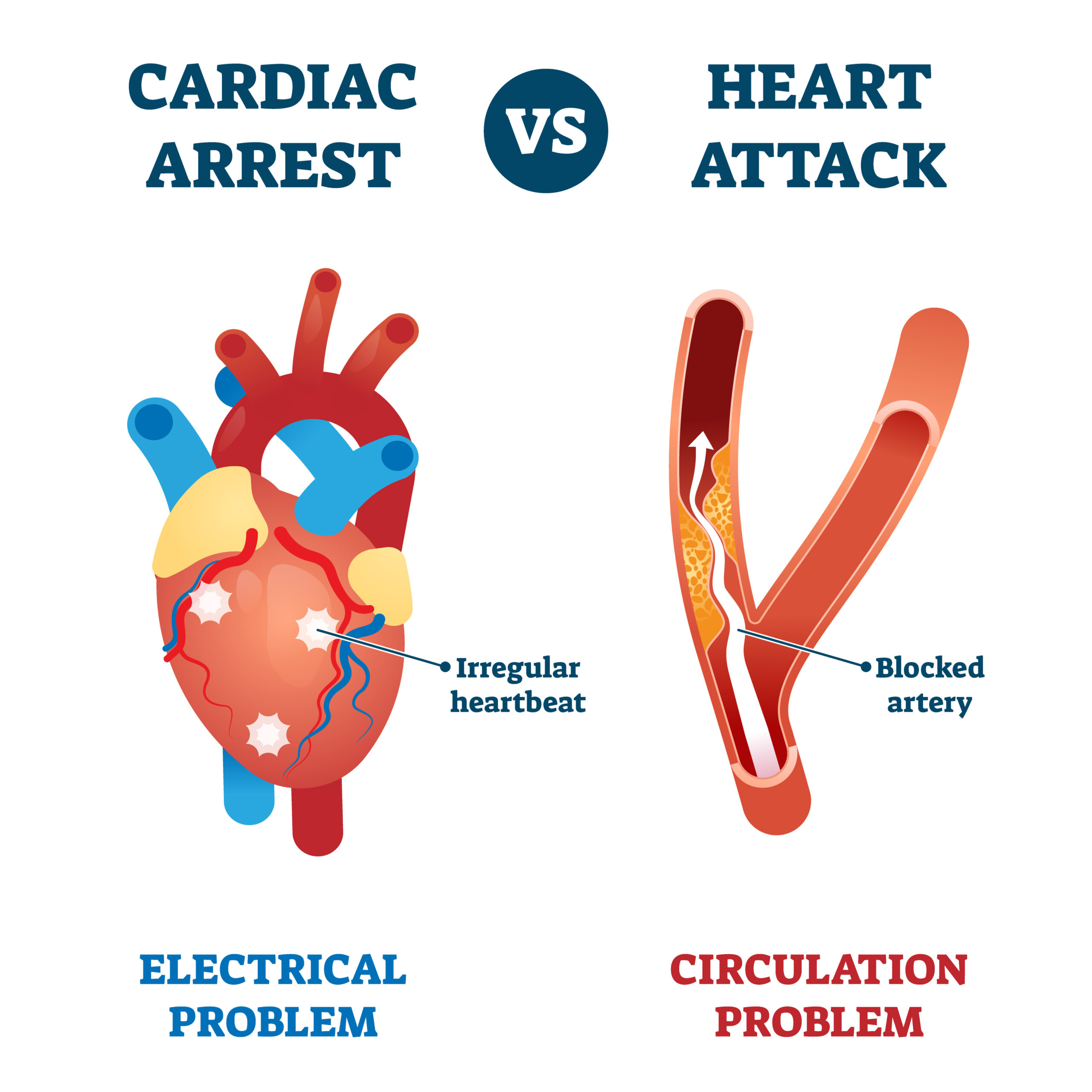
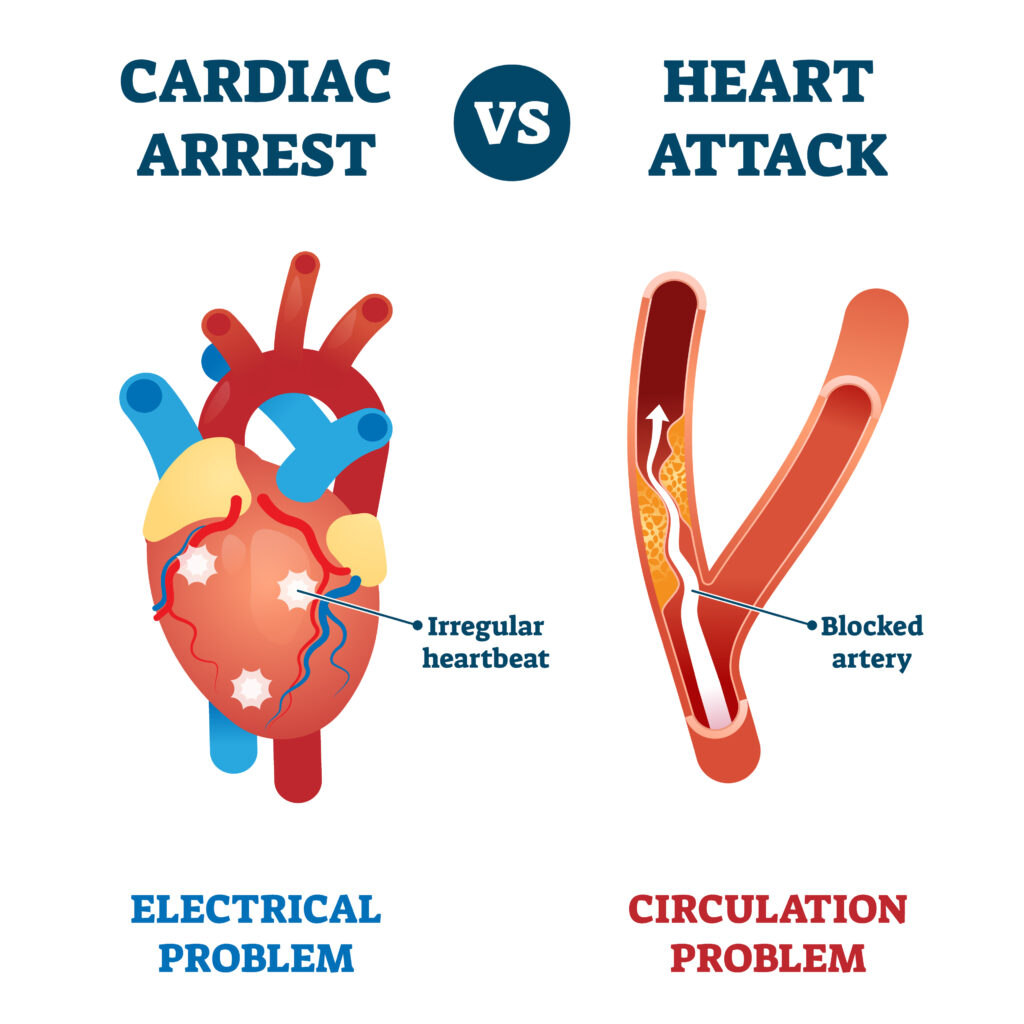
In addition to heart attacks, you may have heard the term cardiac arrest when talking about heart health events. But while these are related, they are actually two very different things.
Let’s uncover the connection and differences between cardiac arrest vs heart attack, including what to look for, what to do if you or someone you know experiences one, and tips for prevention.
What is a Heart Attack?
A heart attack occurs when there’s a partial or total blockage in the artery that brings blood and oxygen to your heart. Arteries can become blocked when fatty deposits called plaque accumulate, restricting blood flow and the transport of oxygen. Without oxygen and essential nutrients, heart muscle cells experience damage or death.
This buildup of plaque is also known as atherosclerosis and happens over time. The good news is that having a heart attack is largely preventable through awareness of your risk factors, practicing healthy lifestyle habits, and working closely with your healthcare team.
Symptoms of a heart attack can include:
- Shortness of breath
- Chest discomfort that lasts more than a few minutes
- Nausea
- Lightheadedness
- Experiencing a cold sweat
- Pain or discomfort in the jaw, stomach, neck, one or both arms
Note that symptoms can vary between men and women. To learn more about heart attacks, including diagnosis, treatment, and prevention, check out my blog post What is a Heart Attack? Facts and Statistics.
What is Cardiac Arrest?
Unlike a heart attack, which is caused by plaque buildup that blocks circulation, cardiac arrest results from an electrical malfunction. This causes your heart to stop beating or to beat so fast that it stops pumping blood.
When someone experiences cardiac arrest, they often collapse, becoming unconscious and unresponsive. Cardiac arrest can happen in someone who may or may not have a diagnosis of heart disease.
Sudden cardiac arrest can also occur. This may either result from an electrical problem or from the heart arteries becoming too clogged with fatty buildup, impeding blood flow.
Additionally, sudden cardiac death is an unexpected death caused by cardiac arrest and loss of heart function. When sudden cardiac arrest occurs, your organs — including your brain and heart — cannot receive oxygen and die without immediate medical attention. Death generally occurs within one hour of onset.
Having other heart conditions, such as cardiomyopathy, arrhythmias, Afib, long Q-T syndrome, and heart failure, can disrupt the heart’s natural rhythm and lead to sudden cardiac arrest.
The Connection Between Cardiac Arrest vs Heart Attack
While heart attacks and cardiac arrest are two distinct events with different causes, they are associated. Most heart attacks don’t cause cardiac arrest, but they can raise the risk, as cardiac arrest can happen following a heart attack or during recovery from one.
What to Do
Heart attacks and cardiac arrest can happen to anyone, anywhere, at any time. This means it’s crucial to know what to do if you or something around you experiences one or both.
If you notice any of the symptoms above in yourself or someone around you, get medical attention right away. Your emergency healthcare providers will conduct a number of diagnostics, including blood tests, to determine what’s going on and devise the best plan forward.
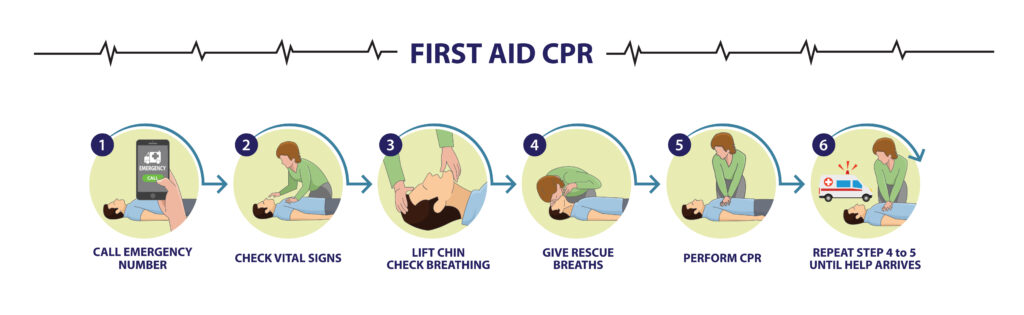
In the meantime, it’s important to know how to administer CPR, or cardiopulmonary resuscitation, in the event that the individual stops breathing. CPR helps to circulate oxygenated blood through the body when the heart is not beating or is beating ineffectively. To find a CPR training class near you, check the American Red Cross website.
Even if you’re unsure, it’s always best to be prudent and seek immediate medical attention anytime you just don’t feel right. It’s better to be checked out and determined to have no urgent medical concerns than to ignore possible symptoms of a life-threatening heart event.
Client Success Story
The best thing you can do to help protect your heart health and reduce your risk of having a heart attack or cardiac arrest is to be aware of your risk factors and take control of them. One of my clients stands out as he had a history of both, multiple risk factors, and wanted to take the lifestyle and nutrition steps needed to protect himself against future problems.
At 63 years old, he came to see me because he was in heart failure (ejection fraction 20%) and he wanted to improve it.
He had previously sustained 2 heart attacks with stent placements and 2 cardiac arrests prior, with a defibrillator in place. He had a history of high blood pressure, high cholesterol, and atrial fibrillation which placed him at high risk for these conditions.
At this time, he was on over 10 medications. He felt lethargic and worn down all day long. He would wake up exhausted and have to come home to take a nap in the middle of the day.
We worked closely together in my VIP intensive program. It was apparent that he was nutrient deficient and had underlying root causes of heart disease from inflammation to insulin resistance. I helped guide him through science-based nutrition and created a personalized health resource guide and meal plan for him. We focused on what to add to his diet in order to optimize his heart function.
In just one month’s time, he had no Afib episodes, his defibrillator never went off, he was off of 2 of his blood pressure medications, and he gained his energy back where he could go the whole day without napping! In 3 months’ time, his cholesterol was optimized (LDL less than 70mg/dL), and his blood sugar levels were optimal (HgA1c less than 5.4%). In 6 months’ time, his ejection fraction went up by 30% to 50%!
He has gained his energy back and feels more confident in his nutrition choices. This should be an empowering story of optimizing heart health, even when faced with multiple risk factors and previous complications.
Tips for Prevention
What’s most important to understand about having a heart attack vs cardiac arrest is how to practice prevention. Optimizing your heart health requires preventive daily lifestyle habits as well as getting regular wellness exams and working closely with your healthcare team including a cardiovascular dietitian to address any risk factors.
- Diet: Heart attacks are caused when plaque builds up in the arteries and restricts or prevents blood flow. It’s important to address the underlying root causes of this — such as inflammation, oxidative stress, insulin resistance, and blood vessel dysfunction — which can largely be improved through science-based nutrition.
For example, one would want to minimize or avoid foods that are known to contribute to plaque formation. This includes foods high in saturated fat, such as eggs, dairy, beef, coconut oil, and palm oil. Instead, focus on foods that are rich in fiber like fruits, vegetables, and whole grains, unsaturated fats like avocado, nuts, and seeds, and nitrates that can open blood vessels, like beets. The therapeutic doses will depend on the individual which is why personalized, science based nutrition is key to results and success.
Furthermore, there is evidence of a strong connection between your gut health and heart health, indicating that some digestive issues can even lead to arrhythmias and atherosclerosis.
- Understanding family and personal health history: Being aware of abnormal heart rhythms in your family can help determine whether you should undergo genetic testing for issues that may cause arrhythmia.
Additionally, being aware of inherited genetic markers, such as high Lipoprotein (a), can help you take a more proactive stance to optimize your lab values. This should be taken into account along with other personal risk factors, such as blood pressure readings and other blood lipids like triglycerides, that you can begin to take under control.
- Improve sleep consistency: Some research has found that people who undergo extreme inconsistencies in their sleep duration are at an increased risk of having a heart attack. Specifically, one 2019 study found that getting fewer than 6 hours or more than 9 hours of sleep per night is associated with a higher heart attack risk independent of other factors.
- Practice stress management: There is evidence that mental stress can promote ventricular fibrillation and arrhythmia which can lead to cardiac arrest. Furthermore, anxiety may play some role in sudden cardiac arrest due to its contribution to other risk factors like heart disease.
Stress is an inevitable part of life, but learning how to minimize its effects on your mental health is key, through things like physical activity, making time for hobbies you enjoy, and communicating with your social support system.
If you’re looking to reduce your risk of having a heart attack or cardiac arrest, I would love the opportunity to meet with you for 1:1 nutrition counseling. Whether you’re living with heart disease risk factors, have had a heart attack, or are otherwise concerned about heart failure, I can help you take the reins of your diet and lifestyle to make positive changes. Schedule a 15 minute complimentary discovery call to discuss more.
References:
- Fang J, Luncheon C, Ayala C, Odom E, Loustalot F. Awareness of Heart Attack Symptoms and Response Among Adults – United States, 2008, 2014, and 2017. MMWR Morb Mortal Wkly Rep. 2019 Feb 8;68(5):101-106. doi: 10.15585/mmwr.mm6805a2. PMID: 31851653; PMCID: PMC6366680.
- Patel K, Hipskind JE. Cardiac Arrest. 2022 Aug 8. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 30521287.
- Kumar A, Avishay DM, Jones CR, Shaikh JD, Kaur R, Aljadah M, Kichloo A, Shiwalkar N, Keshavamurthy S. Sudden cardiac death: epidemiology, pathogenesis and management. Rev Cardiovasc Med. 2021 Mar 30;22(1):147-158. doi: 10.31083/j.rcm.2021.01.207. PMID: 33792256.
- American Red Cross. Training and Certification: Act with Confidence. Available from: https://www.redcross.org/take-a-class
- Yu E, Malik VS, Hu FB. Cardiovascular Disease Prevention by Diet Modification: JACC Health Promotion Series. J Am Coll Cardiol. 2018 Aug 21;72(8):914-926. doi: 10.1016/j.jacc.2018.02.085. PMID: 30115231; PMCID: PMC6100800..
- Rhainds D, Brodeur MR, Tardif JC. Lipoprotein (a): When to Measure and How to Treat? Curr Atheroscler Rep. 2021 Jul 8;23(9):51. doi: 10.1007/s11883-021-00951-2. PMID: 34235598
- Daghlas I, Dashti HS, Lane J, Aragam KG, Rutter MK, Saxena R, Vetter C. Sleep Duration and Myocardial Infarction. J Am Coll Cardiol. 2019 Sep 10;74(10):1304-1314. doi: 10.1016/j.jacc.2019.07.022. PMID: 31488267; PMCID: PMC6785011.
- Chang Liu M, Tester MA, Franciosi S, Krahn AD, Gardner MJ, Roberts JD, Sanatani S. Potential Role of Life Stress in Unexplained Sudden Cardiac Arrest. CJC Open. 2020 Nov 10;3(3):285-291. doi: 10.1016/j.cjco.2020.10.016. PMID: 33778445; PMCID: PMC7984995.
- Batelaan NM, Seldenrijk A, van den Heuvel OA, van Balkom AJLM, Kaiser A, Reneman L, Tan HL. Anxiety, Mental Stress, and Sudden Cardiac Arrest: Epidemiology, Possible Mechanisms and Future Research. Front Psychiatry. 2022 Feb 3;12:813518. doi: 10.3389/fpsyt.2021.813518. PMID: 35185641; PMCID: PMC8850954.