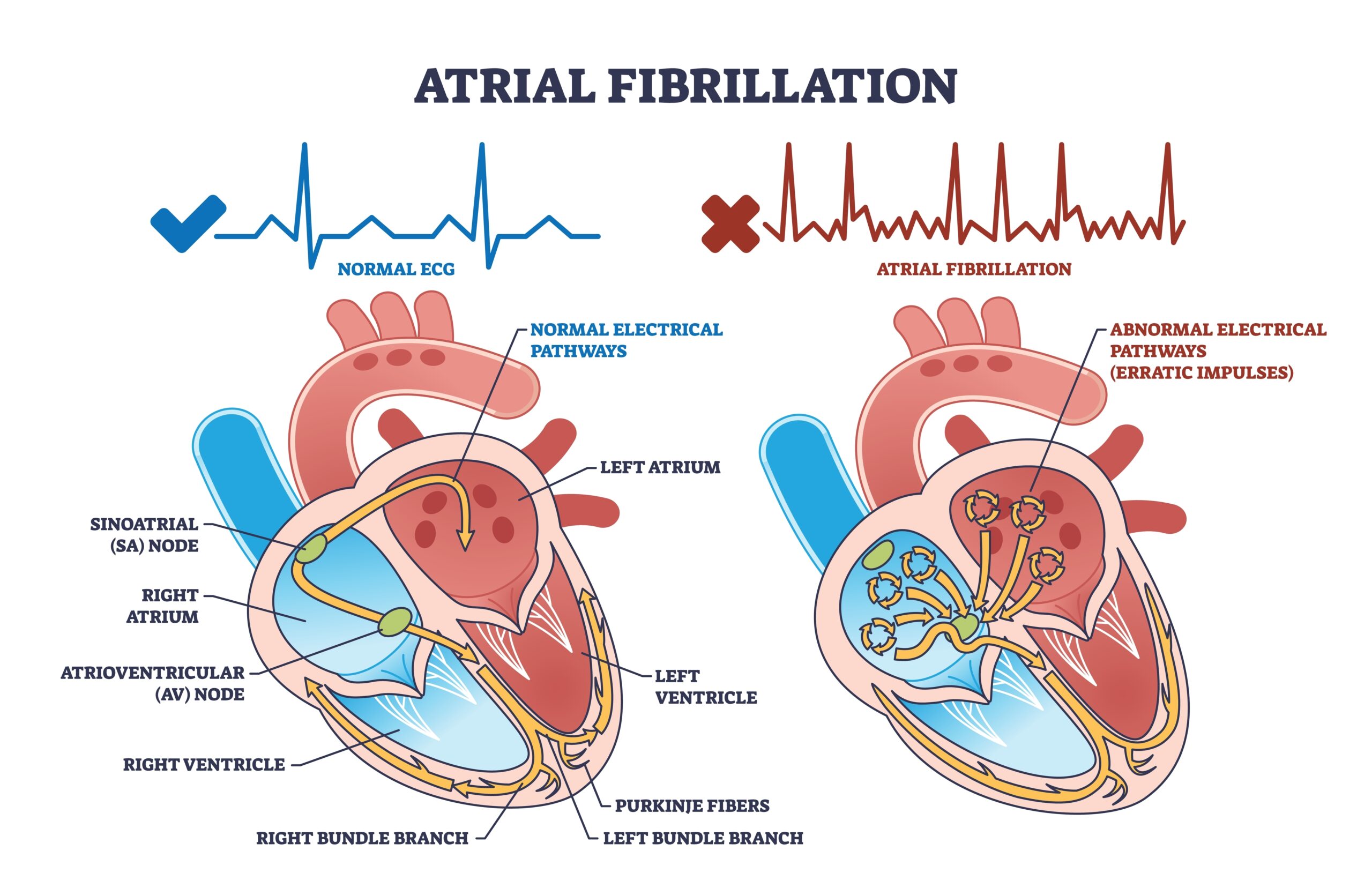
Atrial fibrillation (AFib) is a common heart rhythm disorder that causes the upper chambers of the heart to beat irregularly and often rapidly. This can lead to symptoms like fatigue, shortness of breath, and an increased risk of stroke.
If you’ve been diagnosed with AFib, you may be nervous about continuing your current physical activity routine or exercising more. However, moving your body remains important in caring for your heart and overall wellness, so practicing awareness and safety is key.
We’re covering the benefits, risks, and safest ways to stay active without overdoing it when you’re living with AFib.
Is Exercising with AFib Safe?
Exercising is an important piece of cardiovascular wellness regardless of whether you have existing heart health concerns like AFib. In fact, it’s recommended, while practicing more care than the average person.
Research shows that regular moderate exercise can help manage AFib symptoms, even lowering the frequency and severity of episodes.
One 2020 review of 15 studies involving data from over 1.5 million people found that those who engaged in the recommended physical activity guidelines were at a significantly lower risk of AFib symptoms. Furthermore, studies highlight the benefits of cardiac rehabilitation programs that emphasize exercise for the prevention and treatment of AFib.
Benefits of Exercise for People with AFib
Exercise and AFib can go hand in hand, providing more benefits than risks when it’s done properly and with self-awareness.
Some of the specific benefits include:
- Improved heart function. Staying physically active helps condition your cardiovascular system so that your heart pumps better with less effort. A more efficient heart may be less likely to experience abnormal rhythms.
- Better blood pressure control. High blood pressure can be both a risk factor for and a complication of having AFib. Exercise helps improve vascular health, reducing blood pressure and inflammation. Keeping your blood pressure within normal levels is one of the best ways to reduce your risk of heart attack and stroke related to AFib.
- Enhanced quality of life. Having AFib may make you feel more anxious, tired, or limited in what you can do in your daily life. Exercising can help boost energy, improve your sleep, and reduce AFib symptoms. It can also increase your self-confidence and help you feel more in control.
Risks and When to Be Cautious
Although exercise is generally beneficial when you have AFib, it’s still important to be cautious. There are certain things to watch out for that might indicate a need for workout modifications or a safety break, such as:
- Palpitations or an irregular heartbeat
- Dizziness or lightheadedness, especially during sudden exertion
- Fatigue that feels more intense or sticks around after your workout is over
Other symptoms that indicate a need for emergency attention include:
- Chest pain or pressure
- Shortness of breath that doesn’t resolve with rest
- Fainting
- A sudden spike in heart rate that doesn’t slow down after stopping
- New or worsening palpitations
It’s always best to err on the side of caution, especially if you’re newly diagnosed with AFib or have other heart conditions. Obtaining medical clearance to continue or start an exercise program with AFib can help minimize your risk of serious complications.
Best Types of Exercise for AFib
When you have AFib, consistency and listening to your body are essential. Some of the best ways to get moving safely include:
- Low- to moderate-intensity aerobic exercises, such as walking, cycling, and swimming, for 20-60 minutes several days of the week
- Resistance training focusing on major muscle groups, at least two days per week, using dumbbells, weight machines, or bodyweight
- Be sure to include a proper warm-up and cool-down before and after your workouts to help prepare your heart and muscles for movement.
Afib may require some adjustments to your exercise routine. Starting with low-intensity activities like walking or gentle yoga and spreading movement throughout the day in short sessions can help reduce anxiety around triggering an episode.
Monitor your heart rate and gradually increase intensity as you feel comfortable. Light weights may be more manageable than heavy lifting, especially early on.
Exercising in hot weather adds another layer of stress to the body, so staying hydrated and adjusting your nutrition, particularly electrolytes, can help maintain balance. In fact, combining exercise with supportive nutrition may reduce the frequency or severity of AFib episodes.
Creating a Safe Exercise Plan
The safest way to exercise with AFib is to build a plan alongside your cardiologist or a cardiac rehab specialist. They can help you set appropriate intensity levels and monitor for any concerns.
During workouts, practice self-awareness by keeping an eye on your heart rate and how you feel. Using a fitness tracker or journaling your symptoms can help you stay consistent while identifying patterns.
Client Success Story: AFib and Exercise
Nutrition is a significant component of how to safely exercise with AFib and avoid triggering an episode. A 60-year-old gentleman and athlete came to see me after experiencing a prolonged hospital stay due to an AFib episode. He felt very uneasy about the recurring AFib attacks and wanted to seek nutritional consultation. He had a history of being unable to tolerate medications such as blood thinners, anti-arrhythmics, and statins, despite his doctors’ recommendations.
We worked closely together in my 3-month VIP program, and within 2 weeks, his AFib attacks had stopped. He has now kept AFib in remission for 2.5 months without any medications.
Because he was already physically active, we optimized his nutrition regimen to support heart health and combat oxidative stress. Instead of adding electrolyte supplements, we focused on enhancing his diet with nutrient-dense whole foods rich in calcium, potassium, and magnesium.
We worked on these three main areas:
- Nutrient intake. He was deficient in calcium, potassium, and magnesium. We prioritized getting these nutrients in therapeutic amounts from whole food sources, mindful that calcium and potassium supplementation can sometimes adversely affect the heart. This food-first approach also helped mitigate oxidative stress linked to his athletic activity.
- Gut health. He suffered from acid reflux and constipation, both of which can increase AFib risk. By reducing trigger foods and incorporating therapeutic, gut-friendly foods, we improved his digestion and achieved consistent, healthy bowel movements.
- Insulin resistance. His 43-inch waist circumference indicated possible insulin resistance and inflammation. We targeted this by balancing his meals to stabilize blood sugar and reduce systemic inflammation.
Over the 3 months, he gained more energy, improved sleep, reduced stress, and experienced optimal digestion. He lost 5 inches off his waist and felt more confident about his nutrition choices.
Lifestyle Tips to Support Exercise and AFib Management
Targeted nutrition plays a critical role in supporting a healthy heart rhythm, especially for those managing AFib. The priority should be on nutritional adequacy, getting enough of the essential macro- and micronutrients your body needs to function optimally.
Imbalances in certain electrolytes or even overall caloric intake can disrupt the electrical signals that keep the heart in sinus rhythm. Gut health is also closely linked to heart rhythm stability; issues like bloating, IBS, or microbial imbalance can trigger inflammation and stress responses that may contribute to AFib episodes.
A few healthy lifestyle habits can make exercise safer and more effective when managing AFib include:
- Eat adequate nutrients. Nutrition is central to a stable heart rhythm. Eat adequate amounts of macronutrients and micronutrients for your body to thrive and say in sinus rhythm. Don’t rely on supplements, as drinks and powders can’t replace a nutrient-dense diet. Some may also promote Afib!
- Prioritize sleep. Aim for 7-9 hours of quality sleep, as poor sleep can trigger AFib.
- Manage your stress. While we can’t avoid every stressor, responding to stress with things like deep breathing, prayer, journaling, or yoga can help prevent triggering AFib symptoms.
- Hydrate. Dehydration can disrupt your electrolytes and make your heart work harder. Ditch sugary drinks and sip water throughout the day.
- Approach electrolytes carefully. While electrolyte supplements may be helpful for some, they can contain excessive or unbalanced amounts of sodium, potassium, or magnesium. Talk to your provider before using one.
Pairing exercise with optimal nutrition, hydration, and stress management creates a strong foundation for living well with AFib.
Exercising with AFib: Bottom Line
Having AFib doesn’t mean you have to give up on exercise. Staying active can be one of the most powerful tools for managing your condition. The key is to move mindfully: choose exercises that feel good, listen to your body, and work closely with your healthcare team.
If you want to put Afib in remission through nutrition and lifestyle, I can help. Learn about my 1:1 counseling, group coaching program, or schedule a 15-minute discovery call to see if we’re a good fit.
Sources:
- Leszto K, Frąk W, Kurciński S, et al. Associations of Dietary and Lifestyle Components with Atrial Fibrillation. Nutrients. 2024;16(3):456. Published 2024 Feb 5. doi:10.3390/nu16030456 https://pmc.ncbi.nlm.nih.gov/articles/PMC10856828/
- Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40-43. doi:10.1016/j.sleh.2014.12.010 https://pubmed.ncbi.nlm.nih.gov/29073412/
- Segan L, Prabhu S, Kalman JM, Kistler PM. Atrial Fibrillation and Stress: A 2-Way Street?. JACC Clin Electrophysiol. 2022;8(8):1051-1059. doi:10.1016/j.jacep.2021.12.008 https://pubmed.ncbi.nlm.nih.gov/35981797/
- Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451-1462. doi:10.1136/bjsports-2020-102955 https://pubmed.ncbi.nlm.nih.gov/33239350/
- Leggio M, Fusco A, Coraci D, et al. Exercise training and atrial fibrillation: a systematic review and literature analysis. Eur Rev Med Pharmacol Sci. 2021;25(16):5163-5175. doi:10.26355/eurrev_202108_26530 https://pubmed.ncbi.nlm.nih.gov/34486691/
- Jurado-Fasoli L, De-la-O A, Molina-Hidalgo C, Migueles JH, Castillo MJ, Amaro-Gahete FJ. Exercise training improves sleep quality: A randomized controlled trial. Eur J Clin Invest. 2020;50(3):e13202. doi:10.1111/eci.13202 https://pubmed.ncbi.nlm.nih.gov/31989592/
- Shuai Z, Jie MS, Wen XK, Xu H, Yuan L. Effects of exercise intervention on exercise capacity and cardiopulmonary function in patients with atrial fibrillation: A randomized controlled trial systematic review and meta-analysis. Med Clin (Barc). 2025;164(11):106908. doi:10.1016/j.medcli.2025.106908 https://pubmed.ncbi.nlm.nih.gov/40220475/
- Nesheiwat Z, Goyal A, Jagtap M. Atrial Fibrillation. In: StatPearls. Treasure Island (FL): StatPearls Publishing; April 26, 2023. https://pubmed.ncbi.nlm.nih.gov/30252328/
- Mishima, Ricardo S. et al. Self-reported physical activity and atrial fibrillation risk: A systematic review and meta-analysis. Heart Rhythm, Volume 18, Issue 4, 520 – 528. https://www.heartrhythmjournal.com/article/S1547-5271(20)31165-6/abstract
- Buckley BJR, van Hout L, Fitzhugh C, Lip GYH, Taylor RS, Thijssen DHJ. Exercise-based cardiac rehabilitation for patients with atrial fibrillation: a narrative review. Eur Heart J Open. 2025;5(2):oeaf025. Published 2025 Mar 14. doi:10.1093/ehjopen/oeaf025 https://pubmed.ncbi.nlm.nih.gov/40161304/